Understanding Vocal Shifts and Hormonal Aging
As we age, our bodies undergo a cascade of changes, but one of the most overlooked is the voice. Discover how menopause and andropause impact your vocal folds and what you can do to keep your sound strong.
We often talk about how aging affects our skin, joints, and energy levels, but we rarely discuss the “sound” of aging. Your voice is a finely tuned instrument, powered by a complex interplay of muscles, cartilage, and delicate mucosal tissue. Just as a violin’s wood might change with the seasons, your vocal folds—the two bands of muscle in your larynx—react to the shifting hormonal tides of your body.
If you have noticed that your voice feels “thinner,” your pitch has shifted, or you simply tire out after a long conversation, you aren’t just “getting older.” You are experiencing the physiological impact of hormonal transitions. Whether it is the drop in estrogen during menopause or the gradual decline of testosterone in men, these chemical signals dictate the health and vibration of your voice.
The Science of the Sound: Why Hormones Matter
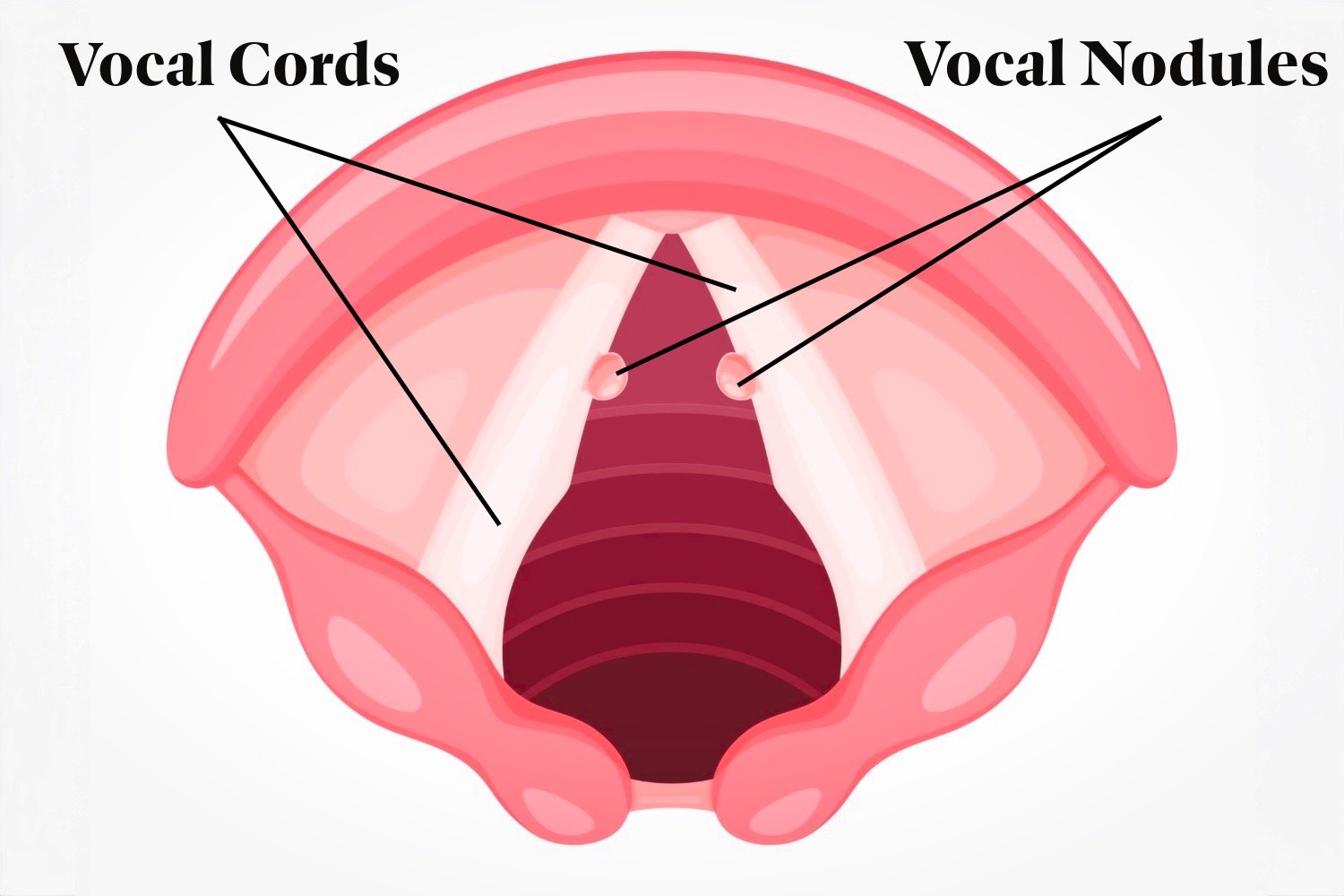
To understand why our voices change, we first have to look at the anatomy of the larynx. The vocal folds are covered in a specialized layer called the lamina propria. This area is rich in proteins like collagen (for strength), elastin (for stretch), and hyaluronic acid (for hydration).
Hormones like estrogen and testosterone act as “maintenance workers” for this tissue. When these hormone levels are high, the vocal folds remain plump, hydrated, and flexible. When they drop, the “maintenance” slows down. The result is a shift in how the vocal folds vibrate, which directly changes the sound the world hears.
The Female Voice: Navigating Menopause
For women, the most significant shift occurs during the perimenopausal and postmenopausal years. This is a period marked by a sharp decline in estrogen and progesterone. In the world of speech-language pathology, we sometimes refer to the resulting symptoms as Menopausal Laryngopathy.
Key Changes in the Postmenopausal Voice
Pitch Lowering: As estrogen levels drop, the vocal folds may become slightly more edematous (swollen) or, conversely, undergo atrophy. For many women, this results in a permanently lower speaking pitch.
Reduced Range: Singers often notice this first. The high notes that used to feel effortless now require significant strain or have disappeared entirely.
Vocal Fatigue: You might find that your voice “gives out” by the end of a dinner party or a long work day.
Dryness: Estrogen helps maintain the mucosal lining of the throat. Without it, the vocal folds can feel “sticky” or dry, leading to a constant need to clear the throat.
An Anecdote: Sarah’s Story
Take “Sarah,” a 52-year-old high school teacher and choir member I recently worked with. Sarah noticed that her “calling voice”—the one she used to command a classroom—felt scratchy and weak. In choir, she found herself shifting from a soprano to an alto because her top notes felt “tight.” By understanding that her vocal folds were losing their natural hydration and elasticity due to menopause, we were able to implement specific resonance exercises to help her find power without the strain.
The Male Voice: The Impact of Andropause
Men also experience hormonal aging, though it is often more gradual. This is sometimes called Andropause. As testosterone levels decline, the primary muscle of the vocal fold (the thyroarytenoid muscle) can begin to lose mass, a process known as sarcopenia.
Key Changes in the Aging Male Voice
Pitch Elevation: Unlike women, whose voices often get lower, men’s voices frequently get higher as they age. This happens because the vocal folds thin out and lose mass, vibrating faster—much like the thin strings on a guitar.
Loss of Projection: Because the vocal folds are thinner and may not close completely (a condition called “bowing”), air escapes during speech. This makes the voice sound breathy or weak.
The “Wavering” Sound: A loss of muscle tone can lead to a slight tremor or instability in the voice, making it harder to sound authoritative.
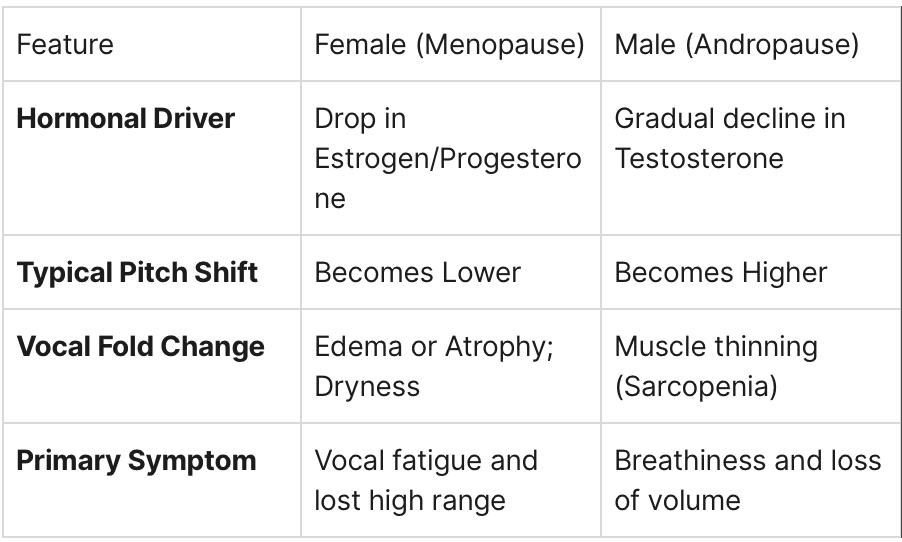
Comparison: Male vs. Female Vocal Aging
Presbyphonia: The Clinical Reality
Regardless of gender, the general medical term for an “aging voice” is Presbyphonia. This is the collective result of hormonal shifts, reduced lung capacity, and the calcification of the laryngeal cartilages.
Think of your voice like a professional athlete. In your 20s, you could “sprint” (scream at a concert or talk for eight hours) without a second thought. As you enter your 50s, 60s, and beyond, your vocal “muscles” require a better warm-up and more intentional recovery. The “athlete” is still there, but the training regimen must change.
How to Protect Your Voice in 2026
The good news is that your voice is highly responsive to therapy and lifestyle adjustments. As we move through 2026, new research continues to show that “voice fitness” is just as important as physical fitness.
1. Hydration is Non-Negotiable
Your vocal folds need systemic hydration to vibrate efficiently. If you are experiencing menopausal dryness, drinking plenty of water and using a personal steamer (nebulizer) can provide direct relief to the tissue.
2. Professional Voice Therapy
Evidence-based programs like PhoRTE (Phonation Resistance Training Exercises) or VFE (Vocal Function Exercises) are designed specifically to “bulk up” aging vocal folds. These are like “weightlifting for your throat” and can help close the gap caused by hormonal thinning.
3. Resonance Training
Learning to “place” your voice in the mask of your face (resonance) reduces the workload on your actual vocal folds. This is the secret to sounding powerful without feeling tired.
4. Consult the Experts
If your voice has changed significantly, it is important to see a Laryngologist (an ENT who specializes in voice) and a Speech-Language Pathologist. They can examine your vocal folds with a tiny camera (stroboscopy) to see exactly how your hormones affect your vibration.
Final Thoughts: Own Your Sound
Your voice is your identity. It carries your history, your emotions, and your authority. While hormonal changes are an inevitable part of the human experience, a “weak” or “old” voice doesn’t have to be. By understanding the science of how estrogen and testosterone maintain our vocal health, we can take proactive steps to keep our instruments in peak performing condition for years to come.
If you are in the Guelph area or looking for virtual support, don’t hesitate to reach out. Your voice has a lot more to say—let’s make sure it’s heard clearly.
Your Voice Recovery Survival Manual
When your voice gives out, every conversation becomes a struggle. Whether you’re a teacher facing another full day of classes, a sales professional with back-to-back calls, or a singer preparing for a performance, vocal strain can derail your entire week. This survival guide walks you through 24 hours of evidence-based home treatment to get your voice back on track.
A Day in the Life of Optimal Vocal Care
I’ve worked with hundreds of professional voice users over the years, and I’ve seen the panic that sets in when their most essential tool suddenly stops working.
Think of your vocal folds like any other muscle in your body. When you strain your hamstring, you don’t just ignore it and run a marathon the next day. Your voice deserves the same respect and recovery protocol.
Morning: The Foundation of Recovery (6:00 AM - 9:00 AM)
Your morning routine sets the tone for the rest of your vocal recovery day. When you wake up, your vocal folds are dehydrated from hours of mouth breathing during sleep. They’re stiff, swollen, and definitely not ready for a presentation at 9 AM.
The Hot Shower Protocol
Start your day with a 10-minute hot shower, but here’s the key: don’t just stand under the water. Turn your bathroom into a steam room by closing the door and letting the mirror fog up completely. The warm, moist air does two critical things. First, it hydrates the superficial layer of your vocal folds, making them more pliable. Second, it helps thin any mucus that’s accumulated overnight, making it easier to clear without the harsh throat-clearing that can cause more damage.
One of my clients, a radio host, swears by adding eucalyptus oil to a washcloth and hanging it near the showerhead. While the aromatherapy is pleasant, remember that the real healing comes from the humidity itself. Keep your mouth slightly open and breathe slowly through your mouth to maximize steam contact with your larynx.
Gentle Neck Stretches
After your shower, when the tissues are warm and pliable, spend five minutes stretching your neck. Tension in neck and shoulder muscles directly affects vocal production. Picture your larynx, or voice box, as resting in a hammock of muscles—if they're tight, everything pulls out of alignment.
Try these stretches in sequence:
Slow head rolls: five in each direction, moving like you’re drawing circles with your nose
Shoulder shrugs: lift to your ears, hold for five seconds, then release with a sigh.
Side neck stretches: ear toward shoulder, hold for 15 seconds each side.
Forward neck stretch: tilt your chin toward your chest, feeling the stretch along your upper back.
The goal isn’t to push into pain. You’re looking for gentle tension release, not a deep tissue workout.
Self-Laryngeal Massage
This technique may feel strange at first, but it is remarkably effective for reducing tension around your voice box. Place your thumb and index finger on either side of your larynx and apply gentle, circular pressure. Work up and down, spending extra time on tight spots.
Think of self-laryngeal massage like soothing a sore shoulder—you’re addressing the external muscles supporting your larynx, not the vocal folds themselves. Spend about three to five minutes on this, and you’ll likely notice swallowing becomes easier and your voice feels less “stuck.”
Mid-Morning: Active Vocal Rehabilitation (9:00 AM - 11:00 AM)
Now that you’ve prepared your voice, it’s time for the real rehabilitation work. This is where Semi-Occluded Vocal Tract Exercises (SOVTEs) become your best friend.
Blowing Bubbles: Your Gateway Exercise
Get a small glass of water and a straw. Take a comfortable breath and blow bubbles steadily for 5-10 seconds. Repeat this 10 times. This simple exercise creates back-pressure, helping your vocal folds vibrate more efficiently with less effort. It’s like doing physical therapy for your voice.
The beauty of bubble blowing is the immediate feedback it provides. If the bubbles are steady and consistent, you’re using good breath support and maintaining even vocal fold vibration. If they’re choppy or you run out of air quickly, you’re working too hard. One teacher I worked with kept a water bottle with a straw at her desk and did bubble exercises between classes. She credited this single habit with ending her chronic voice loss.
SOVTEs: The Heavy Hitters
Move beyond bubbles to these powerful exercises:
Lip trills: blow air through loosely closed lips, making a “motor boat” sound
Tongue trills: roll your R’s if you can, or just let your tongue flutter.
Straw phonation: hum through a straw without water, feeling the vibration in your face
Humming with variation: start low and slide up, then back down smoothly
Do each exercise for 30 seconds, rest for 30 seconds, and repeat five times. These exercises create a therapeutic environment for your vocal folds, allowing them to vibrate with minimal stress.
Midday: Hydration and Environmental Control (11:00 AM - 2:00 PM)
Vocal fold hydration happens in two ways: systemic (drinking fluids) and topical (breathing humid air). You need both for optimal recovery.
The Alkaline Water Advantage
Drink eight to ten glasses of water daily, aiming for at least half as alkaline if available. Alkaline water may help neutralize pepsin, a stomach enzyme that can damage vocal folds during reflux. Pepsin reaches the throat when acid backs up. Even without diagnosed reflux, subtle reflux may underlie many voice issues.
Keep a marked water bottle visible at all times. My rule: if you’re not getting up to use the bathroom every two hours, you’re not drinking enough. One of my physician clients sets hourly phone reminders to drink four ounces—simple but effective.
Herbal Tea Strategy
Sip warm (not hot) herbal tea throughout the afternoon. The warmth provides comfort, and certain herbs offer specific benefits:
Slippery elm: coats and soothes irritated tissue
Marshmallow root: provides mucilage that may help lubricate
Licorice root: has anti-inflammatory properties
Ginger: reduces inflammation and soothes digestive issues.
Add honey for additional coating properties, but skip the lemon if you’re dealing with reflux—the acidity can make things worse.
Nebulizing with Saline
A home nebulizer with sterile saline creates a fine mist that directly hydrates your airway and vocal folds—like irrigation for your voice. Use for 10-15 minutes, two to three times a day.
The investment in a nebulizer (around $30-50) pays off quickly if you’re a professional voice user. I’ve had clients report that 15 minutes with a nebulizer accomplishes what used to take hours of other hydration methods.
Afternoon: Maintaining the Gains (2:00 PM - 6:00 PM)
Environmental Optimization
Your recovery environment matters as much as what you’re actively doing. Run a humidifier in your main workspace to keep ambient humidity between 40-50%. Dry air is your enemy—it strips moisture from your vocal folds faster than you can replace it through drinking.
Position a HEPA air purifier nearby to remove irritants such as dust, pollen, and other particles that can inflame your airways. I learned this lesson from a client who couldn’t figure out why her voice was worse at home than at work—turns out her old HVAC system was constantly circulating allergens.
Modified Voice Use
During recovery, practice “vocal conservation.” This doesn’t mean complete silence, but it does mean:
Speak at a comfortable volume without pushing.
Avoid background noise situations where you must strain to be heard.
Use text or email instead of phone calls when possible.
Take strategic silence breaks between vocal demands.
Avoid whispering, which actually strains your voice more than normal talking.
Evening: Winding Down for Optimal Recovery (6:00 PM - 10:00 PM)
Light Dinner Considerations
Eat your evening meal at least 3 hours before bedtime to minimize your risk of reflux. Avoid common trigger foods like tomato sauce, citrus, caffeine, alcohol, and spicy dishes. Your dinner should be gentle on your digestive system—think lean protein, vegetables, and whole grains.
One corporate trainer I worked with discovered that her chronic morning hoarseness disappeared when she stopped eating after 7 PM. Sometimes the solution is simpler than we expect.
Final SOVTE Session
Do one last round of semi-occluded exercises before bed. This final tune-up helps ensure your vocal folds are in optimal position for overnight healing. Spend 10 minutes on gentle humming, lip trills, and straw exercises. Think of it as tucking your voice in for the night.
Bedtime Preparation
Set up your bedroom for maximum voice recovery:
Run a cool-mist humidifier throughout the night.
Keep a glass of water on your nightstand.
Elevate your head slightly to reduce your risk of reflux.
Ensure your room temperature is comfortable (cooler is generally better)
Remove any irritants, such as strong fragrances or dusty textiles.
If you’re a mouth breather, consider using a chinstrap or working with a sleep specialist. Mouth breathing during sleep is one of the most common but overlooked causes of chronic voice problems.
Steamy Bedtime
The best times to steam your voice are first thing in the morning and right before bed. This is because steam can overrelax the vocal folds, leading to problems when speaking or singing during waking hours. Look for a low-heat vocal steamer or just drape a towel over your head and the steamer bowl, breathe deeply, and let the moisture penetrate. This isn’t just pleasant—it’s therapeutic maintenance that prevents backsliding.
The Reality Check
This full-day protocol represents aggressive home treatment for vocal strain. Most people won’t need to do everything listed here every single day. But when you’re in crisis—when your career depends on your voice, and it’s failing you—this comprehensive approach can make the difference between cancelling commitments and powering through.
I tell my clients to think of this as their vocal emergency kit. You hope you never need it, but when you do, you’ll be grateful you know exactly what to do. Some people can recover with just hydration and rest. Others need the full arsenal. Listen to your voice, respect its limits, and don’t hesitate to seek professional help if you’re not improving after two or three days of intensive home treatment.
Your voice is irreplaceable. Treat it that way, and it will serve you reliably for decades to come.
Speech and Language Development
Speech develops at different speeds, but there are still clear milestones and warning signs. Here’s how to tell what’s “within range,” what may need support, and when speech therapy can help.
Speech development in children (and when therapy is necessary)
If you’ve ever listened to toddlers talk, you know speech can sound like its own language. One day it’s “ba” and “mama,” and the next day it’s a whole story that only a parent can decode. That range is normal, but it also makes it hard to know when to wait and when to act.
Parents often tell me they Googled “speech therapy near me” at 2 a.m. after a well-meaning comment from a relative or a tough daycare drop-off. If that’s you, take a breath. You don’t need to panic to take speech seriously, and you don’t need to “wait and see” if your gut keeps nudging you.
Speech and language are like building a house. Sounds are the bricks, words are the walls, and sentences are the rooms you live in every day. If the foundation is wobbly, we don’t blame the house—we reinforce it, early and steadily, so everything else can grow strong.
This post covers what typical development looks like, what signs suggest that extra support could help, and what actually happens in speech therapy.
Speech vs. language (quick and useful)
People often say “speech delay,” but they may be noticing different things. Speech is how clearly your child makes sounds (like K, S, or R) and how well others can understand them. Language is how your child understands and uses words and sentences to share ideas.
Here are a few everyday examples:
Speech: “tat” instead of “cat,” or “wabbit” instead of “rabbit”
Language: trouble following simple directions, or using very few words to express needs
Social communication: difficulty taking turns in conversation or staying on topic
A child can have challenges in one area and be strong in another, which is why a good assessment matters.
Typical milestones (what many kids do)
There is a wide "normal," but milestones can still guide you. Think of these as signposts, not strict deadlines.
By around 12 months, many children: Recognize their name and familiar words like "no" or "bye-bye." Use gestures like pointing and waving. Say short, simple words, often between 1 and 10.
By around 2 years, many children: Say over 50 words, often more. Begin combining words, like saying "more milk" or "mommy go." Are understood by familiar adults around half of the time.
By around 3 years, many children: Use short sentences to express themselves. Ask simple questions that show curiosity. Are understood by familiar adults most of the time.
By around 4 years, many children: Tell simple stories about their day or interests. Use longer sentences to describe and explain. Are understood by most listeners in most settings.
One helpful rule of thumb for clarity is the “intelligibility guideline”: at 1 year, about 25% understood; at 2, 50%; at 3, 75%; at 4, close to 100% for familiar topics. Kids can still have sound errors at 4, but strangers should usually understand them.
When is therapy necessary? Practical “green, yellow, red” signs
Not every quirk needs therapy. Some kids are late talkers who catch up, while others have mild sound patterns that fade over time. But certain signs suggest it’s worth booking an assessment sooner rather than later.
Green signs:
Your child is learning new words each month
They use gestures, eye contact, and shared attention (like pointing to show you something)
They understand more than they can say
They get frustrated sometimes, but can usually communicate needs
Yellow signs (consider an assessment if they persist):
Limited words for age, or slow vocabulary growth
Speech is hard for people outside the family to understand
Frequent “guessing games” at daycare or school
They avoid talking or let siblings speak for them
Red signs (strong reason to seek help now):
By 12 months: no babbling, no gestures, or not responding to sounds/voices
By 18 months: very few words and limited attempts to communicate
By 2 years: not combining words, or understanding seems limited
Any age: sudden loss of speech/language skills
Strong frustration, frequent meltdowns tied to communication
Stuttering that lasts more than a few months, gets worse, or causes distress
If you’re unsure where your child fits, an assessment can replace worry with a clear plan.
A few “real life” scenarios
To protect privacy, these are blended examples based on common patterns I see in clinic. They may sound familiar.
Scenario 1: “He talks all day at home, but nobody understands him.”
A 3-year-old uses long sentences, but many sounds are missing or swapped. At daycare, peers stop trying to include him in play because they can’t follow his ideas. In therapy, we work on a small set of high-impact sounds, practice them in play, and then coach parents on short daily routines. Clarity improves, and so does confidence.
Scenario 2: “She’s quiet, but she understands everything.”
A 2-year-old follows directions well and loves books, but uses only a few words. Parents are told to wait. Later, frustration increases because she can’t express her choices. Therapy focuses on functional words, simple phrases, and parent strategies that turn daily routines into language opportunities. The goal is not perfect speech overnight—it’s giving her power to communicate.
Scenario 3: “He stutters when he gets excited.”
A preschooler repeats sounds and gets stuck more when tired or rushed. Family members try to help by saying “slow down,” which increases pressure. Therapy teaches parents supportive responses, reduces time pressure, and builds smoother speech patterns. The household feels calmer, and the child speaks more freely.
Common causes (and what speech therapy can and can’t do)
Speech differences can stem from many sources: developmental patterns, hearing history (such as frequent ear infections), motor planning differences, attention and regulation challenges, or broader neurodevelopmental profiles.
Speech therapy does not “force” a child to talk, and it’s not about drilling flashcards for an hour. A good plan is individualized and realistic. It strengthens skills, reduces frustration, and helps families know what to do between sessions.
If there are concerns about hearing, sleep, feeding, or overall development, we may recommend collaborating with your doctor, an audiologist, or other professionals. Team care often helps kids move faster.
What a speech therapy assessment looks like (so it’s less intimidating)
A first visit usually feels more like guided play than a test. Here’s what many pediatric assessments include:
Parent interview (your concerns, milestones, medical and hearing history)
Play-based interaction to observe communication
A speech sound and/or language screening or standardized test (when appropriate)
An oral-motor look (how the mouth moves for speech)
A clear plan: what’s developing, what’s delayed, and what to do next
You should leave with answers in plain language, not a confusing report full of acronyms.
What therapy looks like (and why it works)
For young children, therapy often uses play, movement, books, and routines. The point is practice that transfers into real life.
Depending on your child’s needs, therapy might focus on:
Speech sounds (like K, G, S, or TH)
Early language (first words, combining words, grammar growth)
Understanding language (following directions, concepts like size or location)
Fluency (stuttering support)
Social communication (turn-taking, topic maintenance)
Parents and caregivers are a big part of success. Small daily practice—often 5 to 10 minutes—can matter more than one long session a week.
“Wait and see” vs. “check and support”
Many families get stuck choosing between waiting and jumping in. A middle path is often best: get an assessment, then decide. Some children need direct therapy, some need a short block of parent coaching, and some are fine with monitoring.
Early support can prevent secondary problems such as social withdrawal, behaviour linked to communication frustration, and widening academic gaps as language demands increase in school.
At-home tips you can start today
If you’re on a waitlist or you’re deciding what to do, these strategies are safe and helpful for many kids. Keep them simple and consistent.
Follow their lead in play, then add one step of language (child: “car,” you: “fast car”)
Use “one up” modeling (if they use 1 word, you use 2; if they use 2, you use 3)
Offer choices instead of yes/no (“apple or banana?”)
Pause expectantly (give them time to initiate)
Read the same books repeatedly (repetition builds language fast)
If your child has very limited speech or becomes very distressed, it’s worth getting individualized guidance rather than relying only on generic tips.
Looking for speech therapy in Guelph?
If you’re searching for “speech therapy in guelph,” it helps to choose a clinic that explains the “why” and gives you practical tools for home. A pediatric plan should fit your family’s schedule and your child’s temperament, not the other way around.
If you’ve been typing “speech therapist in Guelph” and wondering who to trust, consider booking an assessment when:
You feel stuck or worried
Others frequently struggle to understand your child
Daycare or school has raised concerns
Your child avoids talking or gets upset when not understood
An assessment doesn’t lock you into long-term therapy. It gives you clarity, options, and a plan.
If you’d like, you can contact our clinic to discuss what you’re seeing and whether an assessment makes sense right now.
Humidity for Vocal Health
Dry indoor air can leave your voice feeling rough, tired, or “stuck.” This guide explains why humidification matters for vocal fold comfort, and how to use nebulizing, steaming, and room or whole-home humidifiers to reduce the effects of surface dryness—especially in winter.
Dry air makes your vocal folds work harder, leading to fatigue, roughness, and that “stuck” feeling that triggers throat clearing. Research shows both systemic hydration (water in your body) and surface hydration (moisture on the vocal fold lining) matter for efficient voice production. Humidification can help mitigate some of the negative effects of surface drying.
Why moisture matters
Vocal folds are not “two strings” that vibrate in open air; they are delicate living tissue that needs a thin, slippery surface layer to move well. When the surface dries out, the tissue can act “stickier,” and studies show dehydration increases the effort needed to start and sustain voicing (often measured as phonation threshold pressure).
A simple way to picture this: rubbing your hands together with a bit of lotion feels smooth, while rubbing them dry feels hot and scratchy. Your vocal folds face a similar problem when the surface layer is dry: more friction, more effort, and less comfort. If you are in Ontario, winter furnace heat can make this a daily issue.
A quick anecdote: a teacher once described her voice as “fine at 8 a.m. and sandpaper by lunch.” Her water bottle was always full, but she was teaching in a warm, dry classroom and mouth-breathing while moving around and talking fast. Once we paired good water habits with targeted humidification, her voice didn’t just sound better; it felt easier to use.
Humidification options that work
Most people do best with a “layered” plan: one method for the room, one for direct moisture, and one for consistency overnight. Clinical voice guidance often includes humidifying inhaled air with devices such as humidifiers, steam inhalation, and nebulizers to support surface hydration.
Below are the main options, with practical pros/cons.
Room (portable) humidifiers
A cool-mist room humidifier is often the easiest starting point because it changes the air you breathe for hours, especially while sleeping.
Best for: overnight dryness, winter furnace heat, waking up with a dry throat.
Pros: Passive support (you don’t have to “do” anything once it’s running).
Cons: Needs regular cleaning; the effect is limited to the room it’s in.
Practical tip: Place it near the bedside, so the mist disperses rather than blowing directly onto your face. If you wake up with a dry mouth, the humidifier helps, but nasal breathing habits and reflux or allergies may also need attention.
Whole-home humidifiers
If the air in every room is dry, which is common in winter, a whole-home humidifier can be a game changer. Think of it like switching from “spot watering one plant” to “installing irrigation.” It’s not as targeted as steam or nebulizing, but the consistency can be excellent for people who use their voice all day.
Best for: households where everyone feels dry, people who work from home, and singers who practice daily.
Pros: Consistent humidity throughout the house; less “room hopping” to find the one humid space.
Cons: Upfront cost, installation, and maintenance.
Steam inhalation (steaming)
Steam is popular with performers because it feels fast and soothing. Professional voice resources discuss using steam inhalers or bedside humidifiers to add external humidification and reduce dryness.
A useful comparison: a humidifier is like setting up a long-term “rainforest environment.” Steaming is like taking your vocal folds on a short visit to a “mini moisture spa.” The effect is temporary, but it can help before or after heavy voice use.
Simple steaming routine (general guidance):
Use a personal steam inhaler or a bowl/mug method with caution.
Aim for warm, comfortable steam—not hot, scalding air.
Keep it short (often 5–10 minutes) and pair it with voice pacing (brief quiet time after heavy use).
Safety note: Steam can burn. If it’s too hot for your face, it’s too hot for your airway.
Nebulizing (nebulized saline)
Nebulizing is different from steaming: instead of warm water vapour, you inhale a cool mist of tiny droplets, often normal saline (0.9%). Research and clinical discussions around vocal fold hydration include nebulizing as one approach to improve superficial (surface) hydration. In a controlled human study, environmental humidification helped return voice effort measures to baseline after a surface dehydration challenge, supporting humidification as a means to reduce the negative effects of superficial drying.
Best for: “my voice feels dry even when I drink water,” winter travel, hotel stays, dry offices, heavy voice weeks.
Pros: Targeted, portable, fast (often 5–10 minutes).
Cons: Requires device care/cleaning; technique matters.
Clinical anecdote: many clients describe nebulizing as the difference between “pushing through the day” and “gliding through the day.” Not because it replaces good technique, but because it reduces the dry friction that makes technique harder to use.
Important: if someone has asthma, chronic lung disease, or tends to experience bronchospasm, it’s worth checking in with a healthcare provider before adding inhaled routines.
How humid should your home be?
More humidity is not always better. Too little humidity can feel harsh on the throat, but too much can increase the risk of mould and dust mites, which can worsen allergies—and allergies can irritate the voice.
Many home and HVAC guidelines point to a comfort/safety range around 30–50% relative humidity, and Canadian-focused sources often cite Health Canada-style recommendations in that neighbourhood as well (with lower targets in winter to reduce window condensation). Some HVAC guidance also discusses an ideal range that can extend higher (such as 40–60%) depending on conditions and goals.
Practical approach (simple and effective):
Buy a small hygrometer (humidity meter).
In winter, start by aiming for 40-45% and adjust based on comfort and condensation.
If windows are dripping with water, humidity is likely too high for that weather and insulation level.
A simple “voice-friendly humidity” plan
If you want an easy plan to follow, try this for two weeks and track how your voice feels (not just how it sounds).
Daily baseline (most voice users)
Morning: Drink water with breakfast (not chugging—just steady intake).
Workday: Add 5 minutes of steam or nebulized saline if you feel dry or you’ll be talking a lot.
Evening: Run a bedroom humidifier overnight if you wake up dry or you live with winter furnace heat.
Heavy voice days (teachers, coaches, sales calls, performers)
Pre-load moisture: 5–10 minutes of steam or nebulizing before the busiest voice block.
Midday reset: 5 minutes of humidification plus 2 minutes of quiet nasal breathing.
Recovery: Humidifier overnight + lighter voice use where possible.
Travel (hotels, planes, conferences)
Air travel and hotels are famously drying. A small travel nebulizer or a simple steam routine can be the “bridge” that keeps your voice stable when your environment is working against you. Pair that with vocal pacing: fewer long calls in echo-y lobbies, fewer “shouted conversations” over restaurant noise, and more short breaks.
When humidification isn’t enough
Humidification supports healthy vibration, but it won’t fix everything on its own. If voice changes are persistent, effortful, painful, or affecting work, it’s worth getting a voice assessment so the plan includes the missing piece (technique, breathing patterns, reflux management strategies, allergy care, workload changes, and, when needed, an ENT evaluation).
Humidification works best when it is part of a bigger goal: making voice use more efficient, more comfortable, and more sustainable, especially through the dry months.
Boost Your Memory and Sharpen Your Mind
Ready to transform your memory and cognitive abilities? This comprehensive guide explores the latest research on memory training, from Cogmed working memory training to photographic memory techniques. Whether you're dealing with mild forgetfulness or seeking peak mental performance, discover the science-backed methods that can help you remember more, think faster, and maintain cognitive health throughout life.
Imagine walking into a room and instantly remembering every detail you see, or effortlessly recalling names and faces weeks after meeting someone. While true photographic memory remains elusive for most of us, the exciting reality is that our memory capabilities are far more trainable than we once believed. Like a muscle that grows stronger with exercise, our cognitive abilities can be enhanced through targeted memory training and strategic brain training memory exercises.
This comprehensive exploration delves into the fascinating world of cognitive training, examining what actually works, what doesn't, and how you can harness proven techniques to sharpen your mental edge. Whether you're a student seeking academic improvement, a professional aiming for peak performance, or someone concerned about mild cognitive impairment, understanding the science behind memory enhancement can transform how your brain functions.
Understanding Memory Training: The Foundation of Cognitive Enhancement
Memory training encompasses a broad range of techniques designed to improve how we encode, store, and retrieve information. Think of your brain as a sophisticated filing system – memory training helps organize those files more efficiently and creates better pathways for accessing them when needed[1][2].
The concept isn't new. Ancient Greek orators used elaborate memory training methods called the "method of loci" to deliver hours-long speeches without notes. Today, neuroscience has revealed why these techniques work so effectively, giving us evidence-based approaches to cognitive enhancement.
Research demonstrates that memory training exercises can produce measurable improvements in cognitive function. A comprehensive meta-analysis found that cognitive training significantly benefited overall cognitive function, with participants showing improvements in delayed memory, orientation, attention, and language skills[3]. However, like learning any new skill, the effectiveness depends heavily on the approach, consistency, and individual factors.
The Science Behind Working Memory Training
Working memory training has emerged as one of the most researched areas in cognitive enhancement. Working memory – our ability to hold and manipulate information in our minds temporarily – is crucial for everything from following complex instructions to performing mental math[4].
Cogmed working memory training, one of the most extensively studied programs, has shown promising results across various populations. Studies involving over 120 research projects demonstrate that participants typically increase their working memory capacity by 0.7 standard deviations – a substantial improvement that allows individuals to outperform a large number of their peers[5][6].
However, the story isn't uniformly positive. A major study called Memory Maestros, involving over 450 students, found that while Cogmed working memory training improved some specific memory tasks, it didn't translate to better academic outcomes[7]. This highlights a crucial distinction in memory training: the difference between near-transfer effects (improvement in similar tasks) and far-transfer effects (improvement in unrelated areas).
One fascinating finding from working memory research is that timing matters significantly. A study from Åbo Akademi University revealed that participants who received a short strategy instruction achieved the same improvements in 30 minutes that typically required a month of training without strategy guidance[8]. This suggests that understanding the "how" behind memory techniques is just as important as practice itself.
Memory Training Apps: Separating Hype from Reality
The digital age has spawned a multi-billion dollar industry of memory training apps and brain training games. Popular platforms like Lumosity, Peak, Elevate, and memoryOS promise to enhance cognitive function through daily exercises[9][10][11].
Recent large-scale research provides a sobering perspective on these claims. A study involving over 44,000 participants found that while brain training showed statistically significant effects, the improvement was small – only 0.06 standard deviations compared to non-users[12]. More tellingly, people who played regular video games showed much larger cognitive improvements (0.47 standard deviations) than those using brain training apps.
However, this doesn't mean all cognitive training apps are worthless. Some studies have shown modest benefits, particularly for older adults with age-related cognitive decline[13][14]. The key is managing expectations and understanding that these apps primarily make you better at the specific tasks they train, rather than providing broad cognitive enhancement.
Best cognitive training apps according to user reviews and research include:
Lumosity: Offers scientifically-designed exercises targeting memory, attention, flexibility, speed, and problem-solving
Peak: Features over 45 games with personalized training programs and coaching features
Elevate: Focuses on practical skills like reading comprehension, grammar, writing, and mathematics
memoryOS: Co-created by a world memory champion, featuring virtual mind palace technology and scientifically proven techniques[9][10][11]
Photographic Memory Training: Myth vs. Reality
The quest for photographic memory training captivates many people seeking cognitive enhancement. True eidetic memory – the ability to recall images with perfect detail – is extraordinarily rare and primarily occurs in young children, disappearing with age[15][16].
However, photographic memory training techniques can dramatically improve visual recall abilities. The most effective approaches include:
Visualization Techniques: Start by observing simple images for 30 seconds, then close your eyes and recreate every detail mentally. Gradually increase complexity as your skills develop[15].
Memory Peg Systems: Associate information with predetermined visual "hooks." For example, linking numbers to vivid images (1 = sun, 2 = shoe) creates memorable connections that facilitate rapid recall[15].
Method of Loci: Also known as the memory palace technique, this involves visualizing familiar locations and placing information in specific spots. World memory champions regularly use this method to memorize thousands of details[15][16].
Chunking Information: Break large amounts of data into smaller, manageable groups. Instead of memorizing "567891234," chunk it into "5678" and "91234" for easier processing[15].
The question "Can you train yourself to have a photographic memory?" has a nuanced answer. While true photographic recall remains elusive, dedicated practice can develop near-photographic abilities for specific types of information. Memory athletes demonstrate this by memorizing entire decks of cards in minutes or recalling thousands of digits of pi[9][16].
Understanding Cognitive Training and Its Applications
Cognitive training extends far beyond simple memory exercises. It encompasses cognitive flexibility training, attention enhancement, processing speed improvement, and executive function development. This broader approach often proves more effective than focusing solely on memory[17][18][19].
Cognitive flexibility training – the ability to switch between different concepts or adapt to changing situations – has shown particular promise. Simple exercises can enhance this crucial skill[20][21]:
Word Games: Scrabble, Bananagrams, and similar games require quick thinking and creative problem-solving
Routine Changes: Taking different routes to work or altering daily patterns stimulates cognitive adaptability
Perspective-Taking: Intentionally viewing situations from others' viewpoints enhances mental flexibility
Logic Games: Chess, Sudoku, and strategy games strengthen flexible thinking patterns[20]
Research indicates that cognitive training programs can be particularly effective when they target multiple domains simultaneously. A meta-analysis of studies involving over 1,000 participants found that multiple cognitive training showed significant effects on attention symptoms and executive function behaviours, while single-domain training often fell short[18].
The Timeline Question: How Long Does Memory Training Take?
One of the most frequently asked questions is “How long does memory training take to show results?”. The answer varies significantly based on the training type, intensity, and individual factors.
For working memory training, research suggests:
Immediate effects: Some improvements visible within 1-2 weeks of consistent practice[22][23]
Significant gains: Typically require 3-5 weeks of regular training (20-25 sessions)[22][24][25]
Long-term benefits: Can persist for years with proper maintenance, though effects may diminish without continued practice[26][27]
A particularly encouraging finding from the ACTIVE study showed that participants who completed at least eight memory training sessions maintained benefits for up to five years, with 80% either maintaining or improving their gains at the one-year follow-up [26][28].
However, training intensity matters significantly. Research comparing high-intensity training (45 minutes, 4 times per week) versus distributed training (45 minutes, 2 times per week) found that the distributed approach produced superior results across multiple cognitive domains [29]. This suggests that consistency trumps intensity in memory training.
Addressing Forgetfulness and Memory Concerns
Forgetting names and experiencing occasional memory lapses are among the most common cognitive complaints. While often dismissed as normal aging, these issues can significantly impact confidence and daily functioning.
Normal vs. Concerning Memory Changes:
Normal age-related changes include occasionally forgetting where you placed your keys, struggling to remember someone's name (but recalling it later), or needing to write more reminders than before[30][31]. These changes are manageable and don't significantly disrupt daily life.
More concerning signs include asking the same questions repeatedly, forgetting common words during conversation, or taking much longer to complete familiar tasks[32]. These symptoms might indicate mild cognitive impairment or other conditions requiring professional evaluation.
Why Am I Forgetting Names All of a Sudden?
Sudden increases in forgetfulness can result from various factors[30]:
Stress and anxiety
Depression
Medication side effects
Sleep deprivation
Hormonal changes
Nutritional deficiencies (particularly B12) Medical conditions affecting brain function
Is Forgetting Names a Sign of Dementia?
Occasional name-forgetting is typically normal, especially when you can recall other details about the person or remember the name later. However, persistent difficulty recognizing familiar people or complete inability to recall names of close family members may warrant medical evaluation[30][32].
Understanding Anomia: When Words Won't Come
Anomia – difficulty retrieving words, particularly names of people, objects, or places – represents a specific type of memory challenge that affects many people[33][34].
Anomia definition: A language disorder characterized by difficulty recalling or producing correct words, especially nouns and verbs, despite understanding their meaning and use[33][34].
Anomia symptoms include:
Pausing mid-sentence while searching for words
Substituting vague terms like "thing" or "stuff"
Describing objects instead of naming them directly
Using hand gestures to demonstrate usage when words fail[33][34]
Types of Anomia:
Word Selection Anomia: Occurs when someone knows how to use an object and can identify it from a group but cannot name it[34].
Semantic Anomia: Involves loss of word meaning, where naming deficits accompany recognition problems[34].
Category-Specific Anomia: Affects particular types of words, such as animals, colors, or tools[34].
Anomia treatment typically involves speech-language therapy focusing on personalized recovery strategies, including cueing techniques, retrieval practice, script training, and customized vocabulary exercises[33].
Mild Cognitive Impairment: Early Intervention Strategies
Mild cognitive impairment (MCI) represents a critical transition state between normal aging and dementia, affecting approximately 10-20% of adults over 65[35][36][37].
Mild cognitive impairment symptoms include[38][37]:
Noticeable memory changes that concern the individual or family
Difficulty with complex tasks requiring multiple steps
Problems with planning and organization
Challenges following instructions or making decisions
Changes in judgment or reasoning ability
MCI vs. Dementia: People with mild cognitive impairment maintain the ability to perform most daily activities independently, while dementia significantly impairs functioning[37].
Types of MCI[37]:
Amnestic MCI: Primarily affects memory, with individuals forgetting important information they previously recalled easily, such as appointments or recent conversations.
Non-amnestic MCI: Affects thinking skills other than memory, including decision-making ability, visual perception, or time/sequence judgment.
Research suggests that cognitive training can be particularly beneficial for individuals with MCI. A recent meta-analysis found significant improvements in global cognitive function, with benefits remaining consistent regardless of training duration[3]. Importantly, cognitive training interventions showed effectiveness whether lasting 2 months or less, 2-6 months, or over 6 months.
Evidence-Based Memory Training Techniques
Based on extensive research, the most effective memory training techniques combine multiple approaches[1][2][24]:
Spaced Repetition: Review information at increasing intervals to strengthen long-term retention. This technique leverages the psychological spacing effect, where distributed practice produces better learning than massed practice.
Active Recall: Instead of passive review, actively test yourself by trying to retrieve information without looking at notes. This process strengthens retrieval pathways and identifies knowledge gaps.
Elaborative Encoding: Connect new information to existing knowledge through personal associations, analogies, or meaningful connections. The richer the association network, the stronger the memory trace.
Multimodal Learning: Engage multiple senses when learning. Combining visual, auditory, and kinesthetic elements creates redundant memory pathways, improving both encoding and retrieval.
Mental Imagery: Create vivid mental pictures of information you want to remember. The brain's visual processing system is exceptionally powerful for memory formation.
Cognitive Behavioral Approaches to Memory Enhancement
Cognitive behavioral therapy training principles can significantly enhance memory training effectiveness. CBT approaches address the psychological barriers that often impede cognitive improvement, such as negative self-talk, performance anxiety, and limiting beliefs about aging and memory capacity[39][40][41].
Online cognitive behavioral therapy training has become increasingly accessible, with programs showing effectiveness comparable to in-person interventions[40][42][41]. These approaches help individuals:
Identify and challenge negative thoughts about memory abilities
Develop realistic expectations for improvement
Build confidence through systematic skill development
Create sustainable practice routines
Manage anxiety related to cognitive performance
The Future of Memory Training: Personalization and Technology
Emerging research emphasizes the importance of personalized approaches to memory training. Individual differences in baseline cognitive ability, learning style, motivation, and life circumstances all influence training effectiveness[1][24][43].
Advanced cognitive training software increasingly incorporates artificial intelligence to adapt difficulty levels, provide personalized feedback, and optimize training schedules for individual users[9]. Virtual reality applications are beginning to show promise for creating immersive memory training environments that more closely approximate real-world challenges[44].
However, technology alone isn't the answer. The most effective approaches combine digital tools with human coaching, social support, and real-world application opportunities[43][45][28].
Practical Implementation: Getting Started with Memory Training
Beginning a memory training journey requires a strategic approach that balances ambition with sustainability. Research suggests that moderate training frequency – 2-3 sessions per week – often produces better results than daily intensive training[18][29].
Setting Realistic Goals:
Start with specific, measurable objectives rather than vague aspirations. Instead of "improve my memory," aim for concrete targets like "remember the names of five new people I meet this week" or "recall my grocery list without writing it down."
Creating a Sustainable Routine:
Consistency matters more than duration. A 15-minute daily practice often produces better results than sporadic hour-long sessions. Consider linking memory exercises to existing habits – practicing recall techniques during your morning coffee or using visualization methods during evening walks.
Tracking Progress:
Document your improvements to maintain motivation and identify effective techniques. Note which strategies work best for different types of information and adjust your approach accordingly.
Real-World Application:
The ultimate test of memory training effectiveness is real-world performance. Deliberately practice newly learned techniques in daily situations – use the memory palace method for your shopping list, apply name-remembering strategies at social events, or employ visualization techniques for work presentations.
Understanding Individual Differences and Limitations
While memory training can benefit most people, individual responses vary significantly. Age, baseline cognitive ability, motivation, and underlying health conditions all influence outcomes[43][46][47].
Age Considerations:
Older adults may require longer training periods to see benefits, but research consistently shows that cognitive training remains effective throughout the lifespan[26][48][49]. The key is adjusting expectations and focusing on personally meaningful improvements rather than absolute performance levels.
Baseline Ability Effects:
Individuals with higher initial cognitive abilities may see different patterns of improvement than those starting from lower baselines[43][47]. This doesn't mean training is less valuable – it simply suggests that goals should be individualized.
Health Factor Impacts:
Conditions like depression, anxiety, sleep disorders, or chronic illness can significantly affect memory training outcomes[50][30]. Addressing these underlying issues often enhances training effectiveness.
The Role of Lifestyle Factors in Cognitive Enhancement
Memory training works best as part of a comprehensive approach to brain health. Research consistently shows that lifestyle factors significantly impact cognitive function and can enhance training benefits[30][51]:
Physical Exercise: Regular aerobic activity increases brain-derived neurotrophic factor (BDNF), promotes neuroplasticity, and improves cognitive performance. Combining physical exercise with cognitive training often produces superior results to either approach alone[51].
Sleep Quality: Adequate sleep is crucial for memory consolidation. Poor sleep undermines training benefits and impairs the brain's ability to form new neural connections.
Nutrition: A Mediterranean-style diet rich in omega-3 fatty acids, antioxidants, and anti-inflammatory compounds supports cognitive function and may enhance training effectiveness.
Social Engagement: Meaningful social interactions provide natural cognitive stimulation and can complement formal training programs.
Stress Management: Chronic stress impairs memory formation and retrieval. Stress reduction techniques like meditation or yoga can enhance training outcomes.
Looking Forward: The Evolving Landscape of Cognitive Enhancement
The field of cognitive training continues to evolve rapidly, with new research regularly refining our understanding of what works, for whom, and under what conditions. Several emerging trends show particular promise:
Precision Medicine Approaches: Future training programs will likely incorporate genetic, biomarker, and neuroimaging data to create highly personalized interventions tailored to individual brain profiles[35][36].
Combination Therapies: Research increasingly supports combining cognitive training with other interventions – physical exercise, pharmacological treatments, or neuromodulation techniques – for enhanced effectiveness[51][52].
Real-World Integration: Rather than isolated training sessions, future approaches will seamlessly integrate cognitive exercises into daily activities, work tasks, and leisure pursuits.
Long-Term Maintenance: Understanding how to maintain cognitive gains over years and decades remains an active area of research, with implications for healthy aging and dementia prevention[26][27].
Conclusion: Your Path to Cognitive Enhancement
The journey of memory training and cognitive enhancement is deeply personal, requiring patience, persistence, and realistic expectations. While we may never achieve the mythical photographic memory, research clearly demonstrates that targeted training can produce meaningful improvements in cognitive function.
The key insights from decades of research point to several crucial principles: consistency trumps intensity, strategy instruction accelerates learning, real-world application ensures transfer, and individual differences matter significantly. Whether you're seeking to sharpen your professional performance, support academic success, or maintain cognitive health as you age, evidence-based memory training offers genuine benefits.
Start small, stay consistent, and remember that cognitive enhancement is not a destination but an ongoing journey. Your brain's remarkable capacity for change and growth – its neuroplasticity – means that it's never too late to begin training your mind for peak performance.
The science of memory training continues to evolve, but one thing remains constant: the human brain's extraordinary ability to adapt, improve, and surprise us with its potential. By applying evidence-based techniques, maintaining realistic expectations, and staying committed to the process, you can unlock new levels of cognitive performance and memory capability.
Whether you choose brain training memory exercises, explore photographic memory training techniques, or focus on working memory training programs, the power to enhance your cognitive abilities lies within your grasp. The question isn't whether memory training works – research has definitively answered that. The question is: are you ready to begin your journey toward a sharper, more capable mind?
***
*Remember: While memory training can produce significant benefits, persistent or concerning memory problems should always be evaluated by healthcare professionals.
Sources
[1] Exploring the effectiveness of a novel memory training program for students with learning disabilities in the United Arab Emirates: investigating the role of gender differences https://www.frontiersin.org/articles/10.3389/feduc.2024.1330906/full[2] The Effect of Memory Training on Cognitive Function: A Systematic Review https://jurnal.globalhealthsciencegroup.com/index.php/IJGHR/article/view/4549[3] A meta-analysis of the consequences of cognitive training ... - PubMed https://pubmed.ncbi.nlm.nih.gov/39233461/[4] Working memory training - Wikipedia https://en.wikipedia.org/wiki/Working_memory_training[5] Benefits of Working Memory Training - Cogmed https://www.cogmed.com/articles/benefits-of-working-memory-training[6] [PDF] Cogmed Working Memory Training - Research Evidents for the ... https://www.pearsonclinical.ca/content/dam/school/global/clinical/us/assets/cogmed/cogmed-claims-and-evidence.pdf[7] Brain training may not be the answer for learning difficulties https://www.mcri.edu.au/news-stories/brain-training-may-not-be-the-answer-for-learning-difficulties[8] One-month worth of memory training results in 30 minutes https://www.abo.fi/en/news/the-outcomes-of-a-month-long-memory-training-can-be-achieved-in-30-minutes-if-the-strategy-is-right/[9] World's Best Memory App to Remember What's Important https://memoryos.com[10] 3 Best Puzzle Games Apps to Sharpen Your Brain in 2025 https://softwarehouse.au/blog/3-best-puzzle-games-apps-to-sharpen-your-brain-in-2025/[11] Brain Training Apps Review: Which one is the best? - Gadget Flow https://thegadgetflow.com/blog/brain-training-apps/[12] A Large-Scale, Cross-Sectional Investigation Into the Efficacy of ... https://pmc.ncbi.nlm.nih.gov/articles/PMC6629869/[13] Brain Training Games Enhance Cognitive Function in Healthy ... https://pmc.ncbi.nlm.nih.gov/articles/PMC5930973/[14] Q&A: Do brain-training apps work? | Mayo Clinic Connect https://connect.mayoclinic.org/blog/take-charge-healthy-aging/newsfeed-post/qa-do-brain-training-apps-work/[15] How to Train Photographic Memory - Smartizen https://smartizen.ca/blogs/news/how-to-train-photographic-memory-proven-techniques-to-sharpen-your-recall[16] How to Develop a Photographic Memory in 7 Days - YouTube https://www.youtube.com/watch?v=Lh3jaiRzQao[17] The relative effectiveness of different combination modes for exercise and cognitive training on cognitive function in people with mild cognitive impairment or Alzheimer’s disease: a network meta-analysis https://www.tandfonline.com/doi/full/10.1080/13607863.2022.2026879[18] Which Factor Is More Relevant to the Effectiveness of the Cognitive Intervention? A Meta-Analysis of Randomized Controlled Trials of Cognitive Training on Symptoms and Executive Function Behaviors of Children With Attention Deficit Hyperactivity Disorder https://www.frontiersin.org/articles/10.3389/fpsyg.2021.810298/full[19] The efficacy of cognitive stimulation, cognitive training, and cognitive rehabilitation for people living with dementia: a systematic review and meta-analysis https://link.springer.com/10.1007/s11357-024-01400-z[20] 10-Minute Flexible Thinking Activities - Life Skills Advocate https://lifeskillsadvocate.com/blog/flexible-thinking-activities/[21] [PDF] Building Cognitive Flexibility - Between Sessions https://www.betweensessions.com/wp-content/uploads/2023/06/Building-Cognitive-Flexibility_050123_ad.pdf[22] Comparison of the Effectiveness of Cognitive Play Therapy and Computer-based Working Memory Training on Impulsivity of Children with Attention Deficit Hyperactivity Disorder in Farsan City https://psj.umsha.ac.ir/article-1-1125-en.html[23] A Study on the Effectiveness of Cognitive Training on Attention, Concentration, Motor Dexterity and Working Memory among Children with Attention Deficit/ Hyperactivity Disorder https://medicopublication.com/index.php/ijphrd/article/view/20333[24] Working Memory Training is Associated with Long Term Attainments ... https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2015.01711/full[25] Effectiveness of Computerized Cognitive Training on Working Memory in Pediatric Cancer Survivors: A Systematic Review and Meta-analysis. https://journals.lww.com/10.1097/NCC.0000000000001348[26] Memory Training in the ACTIVE study: How Much is Needed and ... https://pmc.ncbi.nlm.nih.gov/articles/PMC3825774/[27] Cognitive and hippocampal changes weeks and years after memory ... https://www.nature.com/articles/s41598-022-11636-4[28] What You Need to Know About Cogmed© Working-Memory Training https://www.additudemag.com/cogmed-working-memory-training/[29] Computerised working memory training in healthy adults - PubMed https://pubmed.ncbi.nlm.nih.gov/22671966/[30] Why Do I Keep Forgetting Things? Is It Alzheimer's or Normal Aging? https://www.webmd.com/alzheimers/alzheimers-or-forgetful[31] Memory lapses: Normal or more? - Mayo Clinic Health System https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/memory-lapses-normal-aging-or-something-more[32] Memory loss: When to seek help - Mayo Clinic https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/memory-loss/art-20046326[33] Anomia Treatment That Focuses on Personalized Recovery https://connectedspeechpathology.com/blog/anomia-treatment-that-focuses-on-personalized-recovery[34] Anomic aphasia - Wikipedia https://en.wikipedia.org/wiki/Anomic_aphasia[35] Difference of Cerebrospinal Fluid Biomarkers and Neuropsychiatric Symptoms Profiles among Normal Cognition, Mild Cognitive Impairment, and Dementia Patient https://www.mdpi.com/1422-0067/25/7/3919[36] Systematic Review: microRNAs as Potential Biomarkers in Mild Cognitive Impairment Diagnosis https://www.frontiersin.org/articles/10.3389/fnagi.2021.807764/full[37] Mild Cognitive Impairment (MCI) | Symptoms & Treatments | alz.org https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/mild-cognitive-impairment[38] Mild cognitive impairment - Diagnosis and treatment - Mayo Clinic https://www.mayoclinic.org/diseases-conditions/mild-cognitive-impairment/diagnosis-treatment/drc-20354583[39] Effect of 8 weeks of cognitive behavioral therapy versus 8 weeks core stabilization training in the management of subjects with non-specific low back pain: a randomized controlled trial https://bfpt.springeropen.com/articles/10.1186/s43161-024-00198-3[40] An Online Single-Session Cognitive Behavioral Therapy for Depression and Anxiety Associated with Multiple Sclerosis—Pilot Study https://www.mdpi.com/2076-328X/14/7/620[41] The Fundamentals of CBT: An Interactive Online Course (MGH ... https://lms.mghcme.org/FundamentalsResident[42] Online cognitive behavioral therapy for prolonged grief after traumatic loss: a randomized waitlist-controlled trial https://www.tandfonline.com/doi/full/10.1080/16506073.2023.2225744[43] A Comparison of Computer-based Working Memory Training Effects on Gifted Elementary School Students According to Coaching Methods https://scholar.kyobobook.co.kr/article/detail/4050070346849[44] Virtual Reality Assessment of Classroom – Related Attention: An Ecologically Relevant Approach to Evaluating the Effectiveness of Working Memory Training https://www.frontiersin.org/article/10.3389/fpsyg.2019.01851/full[45] Computerized working memory training for adults with ADHD in a psychiatric outpatient context—a feasibility trial https://www.tandfonline.com/doi/full/10.1080/23279095.2022.2162900[46] The Effectiveness of Working Memory Training for Children With Low Working Memory https://publications.aap.org/pediatrics/article/146/6/e20194028/33544/The-Effectiveness-of-Working-Memory-Training-for[47] Efficacy of cogmed working memory training program in improving ... https://pubmed.ncbi.nlm.nih.gov/34085876/[48] Who would benefit from memory training? A pilot study examining ... https://pmc.ncbi.nlm.nih.gov/articles/PMC3095555/[49] Effectiveness of Computerized Cognitive Training in Delaying Cognitive Function Decline in People With Mild Cognitive Impairment: Systematic Review and Meta-analysis https://www.jmir.org/2022/10/e38624[50] Anticholinergic burden for prediction of cognitive decline or neuropsychiatric symptoms in older adults with mild cognitive impairment or dementia. http://doi.wiley.com/10.1002/14651858.CD015196[51] Effectiveness of combined physical exercise and cognitive training in older adults with cognitive impairment: A systematic review and meta-analysis https://narraj.org/main/article/view/1040[52] The Effectiveness of Computerized Cognitive Training in Patients With Poststroke Cognitive Impairment: Systematic Review and Meta-Analysis https://www.jmir.org/2025/1/e73140
Unlocking Your Brain's Hidden Potential: Language-Based Cognitive Training
Speech-language pathologists are uniquely positioned to help healthy teens, adults, and seniors with mild cognitive impairment enhance their cognitive abilities through targeted language-based training programs that harness the brain's natural ability to adapt and grow.
The Brain's Amazing Ability to Change
Picture your brain as a bustling city. Every day, new roads are built while old ones are repaired. This amazing process, called neuroplasticity, means your brain can create new pathways throughout your entire life[1][2][3]. Just like a muscle grows stronger with exercise, your brain becomes sharper with the right training.
Speech-language pathologists (SLPs) understand this powerful concept better than most. They work with people every day who need to rebuild their thinking skills after injury or illness[1][4]. However, these same techniques can help healthy people too. Think of it as going to the gym for your brain.
The exciting news is that cognitive training isn't just for people with brain injuries anymore. Research shows that healthy teens, adults, and seniors can all benefit from these programs[5][6][7]. It's like having a personal trainer for your mind.
Who Benefits from Cognitive Training?
Healthy Teenagers: Building Strong Foundations
Teenagers have brains that are still developing. This makes them perfect candidates for cognitive training[8][9]. During adolescence, the brain goes through major changes. It's like a construction site where important connections are being built.
Studies show that teens who participate in cognitive training programs improve their attention, memory, and problem-solving skills[6]. One research study found that high school students who did brain training exercises for just four months showed better performance in all cognitive areas[8]. The key was making sure the exercises were challenging enough to really work their brains.
Consider Sarah, a 16-year-old student who struggled with focus during class discussions. After working with an SLP on attention training exercises, she began participating more actively in debates. Her teachers noticed she could follow complex conversations and remember important details much better than before.
Healthy Adults: Staying Sharp
Adults face unique challenges in our fast-paced world. Work stress, multitasking, and information overload can make anyone feel mentally foggy. Language-based cognitive training offers a solution that's both practical and effective[4][10].
Adult brains benefit from exercises that combine physical activity with mental challenges[11][12]. It's like doing a workout that trains both your body and mind at the same time. Research from Western University found that adults who combined exercise with cognitive training showed much better results than those who did either activity alone[11].
Mark, a 45-year-old executive, found himself forgetting important details during meetings. He worked with an SLP who designed a program that included memory exercises and communication strategies. Within three months, Mark reported feeling more confident at work and could handle complex projects with greater ease.
Seniors with Mild Cognitive Impairment: Maintaining Independence
For seniors experiencing mild cognitive impairment (MCI), cognitive training can be life-changing[13][14]. MCI sits between normal aging and dementia. People with MCI notice changes in their thinking, but they can still live independently[15][13].
SLPs help seniors with MCI by focusing on practical skills they need every day[14][16]. These might include remembering medication schedules, following recipes, or keeping track of appointments. The goal is to help people stay independent as long as possible.
Consider Robert, a 72-year-old retired teacher who began having trouble remembering his grandchildren's names. His family was worried, but an SLP assessment showed he had MCI rather than dementia. Through targeted training exercises, Robert learned strategies to improve his word-finding abilities. Six months later, he was back to telling detailed stories about his teaching days.
How Language-Based Training Works
The Connection Between Language and Thinking
Language and thinking are deeply connected in your brain[4][17]. When you struggle to find the right word, it often reflects broader thinking challenges. SLPs understand this connection better than anyone. They know that improving language skills often improves overall cognitive function.
Think of language as the highway system in your brain. When traffic flows smoothly, everything works better. But when there are roadblocks or detours, the whole system slows down. SLPs help clear these roadblocks through targeted exercises.
Evidence-Based Techniques
Modern cognitive training uses techniques backed by solid research[18][19]. SLPs don't just guess what might work. They use proven methods that help the brain build new connections and strengthen existing ones.
One effective approach is called "retrieval practice"[20]. Instead of just reading information over and over, people practice recalling it from memory. It's like the difference between highlighting a textbook and taking practice tests. The practice tests make your brain work harder, which leads to better learning.
Another technique involves "dual-task training"[21]. This means doing two things at once, like walking while doing memory exercises. It sounds simple, but it's actually quite challenging for your brain. This type of training helps improve divided attention, which is crucial for daily life activities.
Personalized Programs
Every person's brain is unique, just like their fingerprints. What works for one person might not work for another[18]. That's why SLPs create individualized programs based on each person's specific needs and goals.
For example, a teenager might focus on attention and working memory to improve school performance. An adult might work on processing speed and multitasking abilities for better job performance. A senior with MCI might concentrate on memory strategies and word-finding techniques to maintain social connections.
Real-World Success Stories
The Power of Persistence
Lisa, a 28-year-old graduate student, felt overwhelmed by her coursework. She couldn't concentrate during long lectures and forgot important details from her reading. Her SLP designed a program that included attention training exercises and reading comprehension strategies.
At first, the exercises felt difficult and frustrating. Lisa compared it to learning to play piano as an adult - everything felt awkward and slow. However, after eight weeks of consistent practice, she noticed significant improvements. She could focus during two-hour seminars and remember complex research findings much better.
The key to Lisa's success was consistency. Like going to the gym, cognitive training requires regular practice to see results. Lisa practiced her exercises for 30 minutes each day, five days a week. The routine became as natural as brushing her teeth.
Family Involvement Makes a Difference
Tom, a 68-year-old with early MCI, initially resisted the idea of cognitive training. He felt embarrassed about needing help with his thinking skills. However, his wife encouraged him to try working with an SLP.
The SLP involved Tom's wife in the training process. She learned how to support Tom's practice at home and recognize signs of progress. This team approach made a huge difference. Tom felt less alone in his journey, and his wife felt empowered to help.
After six months of training, Tom showed significant improvements in his memory tests. More importantly, he felt more confident in social situations. He started playing bridge again with his friends and even began volunteering at the local library.
The Science Behind Success
Neuroplasticity in Action
Recent brain imaging studies show exactly how cognitive training changes the brain[22][23]. When people participate in intensive language-based training, their brains literally rewire themselves. New connections form between brain cells, and existing connections become stronger.
This process happens at any age, though it might take longer in older adults[24]. It's never too late to improve your brain function. Think of it like renovating an old house - with the right tools and techniques, you can make significant improvements regardless of the building's age.
The Role of Challenge and Support
Effective cognitive training follows what researchers call the "Goldilocks principle" - not too easy, not too hard, but just right[23]. If exercises are too simple, your brain doesn't work hard enough to change. If they're too difficult, you become frustrated and give up.
SLPs are experts at finding this sweet spot. They gradually increase the difficulty of exercises as your skills improve. It's like a video game that gets harder as you level up. This progressive challenge keeps your brain engaged and growing.
Practical Applications
School and Work Performance
Cognitive training has real benefits for academic and professional success[6]. Students who participate in these programs often see improvements in their grades and test scores. Working adults report better job performance and less mental fatigue at the end of the day.
The skills learned in cognitive training transfer to real-world situations. For example, attention training helps students focus during lectures and working adults concentrate during long meetings. Memory exercises help people remember important information without constantly checking their notes.
Daily Life Independence
For seniors with MCI, cognitive training can mean the difference between living independently and needing additional care[14][16]. The exercises help people maintain the thinking skills they need for daily activities like cooking, managing money, and taking medications safely.
This independence has emotional benefits too. People feel more confident and less anxious when they trust their thinking abilities. Family members also feel less worried when their loved ones can handle daily tasks safely.
Looking to the Future
The field of cognitive training continues to evolve rapidly. New technologies like virtual reality and computerized programs are making training more engaging and accessible[25][26]. However, the human touch provided by SLPs remains crucial for success.
Research shows that the most effective programs combine high-tech tools with human guidance[18]. SLPs provide the expertise needed to design appropriate programs and the support needed to maintain motivation. They're like personal trainers for your brain.
The future looks bright for people seeking to improve their cognitive abilities. As our understanding of neuroplasticity grows, training programs become more effective and efficient. What once seemed impossible - significantly improving brain function in healthy adults - is now a reality.
Taking the First Step
If you're interested in cognitive training, the first step is talking with a qualified SLP. They can assess your current abilities and design a program that meets your specific needs and goals. Remember, improving your brain function is a journey, not a destination.
Like any worthwhile endeavor, cognitive training requires commitment and patience. However, the rewards - better memory, sharper attention, and improved confidence - make the effort worthwhile. Your brain has amazing potential waiting to be unlocked. With the right guidance and training, you can tap into abilities you never knew you had.
[1] Cognitive Speech Therapy https://www.betterspeech.com/lp/cognitive-speech-therapy[2] Harnessing Neuroplasticity for Language Recovery https://www.numberanalytics.com/blog/neuroplasticity-language-recovery[3] Unlocking the Power of Neuroplasticity - Caroline Bowen https://speech-language-therapy.com/media/pgs/unlocking-neuroplasticity.html[4] How Speech Therapy Supports Cognitive Function - VoxLingue https://www.voxlingue.com/post/speech-therapy-cognitive-function-montreal[5] Brain Training Games Enhance Cognitive Function in Healthy ... https://pmc.ncbi.nlm.nih.gov/articles/PMC5930973/[6] Effects of physical activity interventions on cognitive outcomes and ... https://www.tandfonline.com/doi/full/10.1080/02640414.2020.1794763[7] Cognitive Training For Older Adults https://acognitiveconnection.com/cognitive-training-for-older-adults/[8] Exercise, Cognition, and the Adolescent Brain - PMC https://pmc.ncbi.nlm.nih.gov/articles/PMC5973814/[9] Navigating Cognitive Health in Teens and Young Adults: Early ... https://www.drcognitivehealth.com/blog/navigating-cognitive-health-in-teens-and-young-adults-early-intervention-strategies[10] The Benefits of Cognitive Speech Therapy for Adults https://connectedspeechpathology.com/blog/enhancing-communication-the-benefits-of-cognitive-speech-therapy-for-adults[11] New study finds exercise, cognitive training combo boosts mental ... https://www.schulich.uwo.ca/about/news/2023/august/synergic-rct.html[12] New study finds exercise, cognitive training combo boosts mental ... https://www.sjhc.london.on.ca/research/stories/new-study-finds-exercise-cognitive-training-combo-boosts-mental-sharpness-seniors[13] Improving Practices for Mild Cognitive Impairment and Early-Stage ... https://pmc.ncbi.nlm.nih.gov/articles/PMC9531927/[14] Understanding SLP Interventions For Those Living With MCI https://foxrehab.org/mild-cognitive-impairment-progression-speech-language-pathology/[15] Overcoming Mild Cognitive Impairment with Speech Therapy https://www.physioinq.com.au/blog/overcoming-mild-cognitive-impairment-with-speech-therapy[16] 20Q: Mild Cognitive Impairment - The SLP's Role in Service Delivery https://www.speechpathology.com/articles/20q-mild-cognitive-impairment-slp-20571[17] Connected Speech and Language in Mild Cognitive Impairment and ... https://pmc.ncbi.nlm.nih.gov/articles/PMC6198327/[18] American Speech-Language-Hearing Association Clinical Practice ... https://pubs.asha.org/doi/10.1044/2022_AJSLP-21-00361[19] Cognitive Intervention Strategies Directed to Speech and Language ... https://pmc.ncbi.nlm.nih.gov/articles/PMC8533834/[20] [PDF] Evidence-Based Review of Moderate to Severe Acquired Brain Injury https://erabi.ca/wp-content/uploads/2018/12/Ch7_V12_cog-com.pdf[21] What SLPs Need to Know: Treating Attention in Speech Therapy https://tactustherapy.com/treating-attention-in-speech-therapy-slp-cognition/[22] Neuroplasticity and Functional Recovery after Intensive Language ... https://pmc.ncbi.nlm.nih.gov/articles/PMC5487528/[23] Neuroplasticity of Language Networks in Aphasia - PubMed Central https://pmc.ncbi.nlm.nih.gov/articles/PMC6454116/[24] Long-term studies in cognitive training for older adults https://pmc.ncbi.nlm.nih.gov/articles/PMC9173785/[25] Cognitive Stimulation Therapy Program For Adults https://www.northernspeech.com/stroke/leap-a-science-based-clinician-ready-cognitive-stimulation-program-for-adults/[26] Using Speech Therapy Apps to Treat Cognitive-Communication ... https://tactustherapy.com/cognitive-communication-apps/Executive Dysfunction, Working Memory, and the Episodic Buffer
The episodic buffer plays a crucial role in how we process and integrate information during communication. When this working memory component is impaired, it can significantly affect an adult's ability to engage in meaningful conversations, follow complex instructions, and express coherent thoughts.
This article provides a comprehensive examination of various cognitive processes that influence communication. If it’s been a while since PSY 101, or you’re new to this topic, here’s a quick glossary of terms to help get the most out of this article:
Executive functions: They form the control center of the brain. Collectively, these functions enable individuals to mentally explore ideas, take the time to think before acting, meet new and unanticipated challenges, resist temptations, and stay focused. The three main executive functions are:
Inhibitory Control: The ability to control attention, behaviour, thoughts, and emotions to override impulses or distractions
Cognitive Flexibility: The ability to switch perspectives, adapt to new rules, or think creatively
Working Memory: The ability to hold information in mind and mentally work with it. It comprises three distinct forms, including:
Phonological loop—working memory for sound
Visuospatial sketchpad—working memory for visualization
Episodic buffer—working memory that helps integrate and organize perceptions and long-term memory into sequences, or “episodes”
This article examines the episodic buffer and its connection to communication, particularly in relation to narrative and storytelling skills.
What is the Episodic Buffer?
Jessica (name changed for privacy) sat across from me during our first session, her frustration evident as she struggled to tell me about her weekend. She could remember individual details—the restaurant name, what she ordered, who she was with—but weaving these pieces together into a coherent story seemed impossible. Her words came in fragments, jumping between topics without the smooth integration that typically characterizes natural conversation. What Sarah was experiencing wasn't just a memory problem; it was a breakdown in her episodic buffer, a critical component of working memory that serves as the bridge between different types of information processing.
The episodic buffer represents one of the most fascinating and complex aspects of human cognition. First proposed by psychologist Alan Baddeley in 2000, this component of working memory acts as a temporary storage system that integrates information from multiple sources into coherent, unified representations. Think of it as a mental workspace where different types of information—what you hear, see, remember, and think—come together to form meaningful experiences.
Unlike other components of working memory, which handle specific types of information (such as the phonological loop for sounds or the visuospatial sketchpad for visual information), the episodic buffer is uniquely equipped to bind different elements together. This binding process allows us to create rich, contextual memories and communicate complex ideas that draw from multiple sources of information simultaneously.
The Orchestra Analogy
Imagine an orchestra where each musician represents a different type of information processing. The phonological loop might be the string section, processing the sounds and rhythms of language. The visuospatial sketchpad could be the brass section, handling visual and spatial information. The episodic buffer, then, serves as the conductor—not making music itself, but ensuring all the different sections work together harmoniously to create a unified performance.
When the episodic buffer functions properly, our communication flows naturally. We can tell stories that weave together what we saw, heard, felt, and remembered. We can follow complex conversations that jump between topics while maintaining the overall thread. However, when this system breaks down, the result can be fragmented and disjointed communication, leaving both the speaker and the listener frustrated.
How Episodic Buffer Dysfunction Affects Communication
Many otherwise healthy adults often struggle with tasks that require the episodic buffer to integrate multiple sources of information. Research has shown that working memory deficits, particularly in the episodic buffer, can significantly impact language abilities. This connection between working memory and communication becomes especially apparent in several key areas:
Story Coherence and Narrative Skills
One of the most noticeable effects of episodic buffer dysfunction is difficulty creating coherent narratives. Take Marcus, a 54-year-old client who complained about his difficulty telling personal narratives. While he had an excellent vocabulary and a good memory for details, he struggled to tell connected stories about his experiences. While hosting friends for dinner, he struggled to tell a story about his daughter’s recent wedding. He could remember the events of the day, that it was beautiful, and that he gave a speech, but connecting these elements into a flowing narrative proved challenging.
This difficulty stems from the episodic buffer's role in binding temporal and contextual information. When this system is impaired, individuals may remember the facts (semantic memory) but struggle to organize them into the rich, contextual episodes that make for engaging storytelling.
Following Complex Instructions
The episodic buffer also plays a crucial role in following multi-step instructions, particularly those that require integrating new information with existing knowledge. Consider the difference between these two instructions:
Simple: "Take the blue folder to the office."
Complex: "Take the blue folder that contains the Johnson report to the office on the second floor, but first make sure to remove any documents marked 'confidential' and file them in the secure cabinet."
The second instruction requires the episodic buffer to hold and integrate multiple pieces of information while executing the task. Adults with episodic buffer dysfunction may struggle with such complex instructions, not because they don't understand the individual components, but because they are unable to maintain and coordinate all the elements simultaneously.
Conversational Turn-Taking
Effective conversation requires constant integration of what we want to say with what others have said, adjusting our responses based on contextual cues and maintaining awareness of the overall conversational flow. Research has shown that adults with communication disorders often exhibit slower speech rates and delayed turn-taking, which may reflect the additional cognitive load required when the episodic buffer isn't functioning optimally.
The Episodic Buffer Across Different Communication Disorders
Mild Cognitive Impairment and Dementia
In conditions like mild cognitive impairment (MCI) and early-stage dementia, episodic buffer dysfunction often manifests as difficulty with autobiographical memory and personal narrative. Research indicates that language performance deficits can appear early, even before impairments in episodic memory become apparent. This suggests that the episodic buffer's role in language processing may be particularly vulnerable in neurodegenerative conditions.
Adults with MCI often report feeling like they're "losing their words" or having trouble organizing their thoughts. What they're experiencing isn't simply a vocabulary problem—it's a breakdown in the system that helps integrate and organize information for communication.
Autism Spectrum Disorder
Interestingly, research has revealed similarities between autism spectrum disorder (ASD) and healthy aging in terms of episodic buffer function. Both populations may struggle to create unified representations of individual event features, resulting in fragmented communication patterns.
Adults with ASD might excel at remembering specific details but struggle to integrate these details into coherent social narratives. This can affect their ability to engage in the kind of contextual, relationship-building communication that relies heavily on episodic buffer function.
ADHD and Working Memory
While research suggests that the episodic buffer may be relatively intact in ADHD, the interaction between attention difficulties and working memory can still impact communication. Adults with ADHD might have the capacity to integrate information but struggle to maintain focus long enough for the episodic buffer to function effectively in complex communication situations.
Assessment and Clinical Implications
Recognizing Episodic Buffer Dysfunction
Speech-language pathologists are uniquely positioned to identify episodic buffer dysfunction through careful observation of communication patterns. Key indicators include:
Fragmented storytelling: Ability to recall details but difficulty weaving them into coherent narratives
Context-switching difficulties: Struggles when conversations shift topics or require integration of multiple themes
Instruction-following challenges: Particular difficulty with multi-step or conditional instructions
Conversational repair difficulties: Trouble using context to resolve misunderstandings
Assessment Tools and Approaches
Modern assessment batteries are beginning to incorporate episodic buffer evaluation more systematically. The Arizona Battery for Communication Disorders of Dementia (ABCD), for example, evaluates multiple aspects of cognition, including episodic memory and linguistic comprehension. More recent developments, such as the REMEDES battery, are specifically designed to assess working memory components, including episodic buffer recruitment.
However, assessment shouldn't rely solely on formal testing. Ecological assessment—observing how individuals function in real-world communication situations—provides crucial insights into episodic buffer function that standardized tests might miss.
Treatment Approaches and Interventions
Working Memory Training
Recent research has shown promising results for working memory programs that target episodic buffer function. These programs typically include activities that require integrating information from multiple sources, such as:
Multi-modal story retelling: Combining visual, auditory, and textual information
Complex instruction following: Gradually increasing the complexity of multi-step tasks
Contextual conversation practice: Structured activities that require maintaining and integrating conversational themes
Compensatory Strategies
For individuals with persistent episodic buffer dysfunction, compensatory strategies can significantly improve communication effectiveness:
External memory aids: Using visual organizers, digital tools, or written notes to support integration
Chunking techniques: Breaking complex information into smaller, manageable pieces
Rehearsal strategies: Practicing the integration of information before communication attempts
Environmental Modifications
Creating communication environments that reduce episodic buffer demands can improve success:
Reducing distractions: Minimizing competing information that might overload the system
Providing context cues: Using visual or verbal reminders to support integration
Structured conversation formats: Implementing predictable patterns that reduce cognitive load
The Future of Episodic Buffer Research
As our understanding of the episodic buffer continues to evolve, several exciting research directions are emerging. Neuroimaging studies are beginning to identify the brain regions involved in episodic buffer function, which may lead to more targeted interventions. Additionally, research into the relationship between episodic buffer function and everyday communication participation is helping us understand the real-world impact of these cognitive processes.
Implications for Families and Caregivers
Understanding episodic buffer dysfunction can help families and caregivers better support their loved ones with communication disorders. Rather than focusing solely on what someone can't remember or say, recognizing the integration challenges can lead to more effective support strategies.
For example, instead of asking open-ended questions like "How was your day?" caregivers might provide more structured prompts: "I know you went to the store this morning and then had lunch with your sister. Can you tell me about one of those activities?" This approach provides the contextual framework that the impaired episodic buffer struggles to create independently.
Conclusion
The episodic buffer represents a crucial but often overlooked component of communication function. By understanding how this system integrates information from multiple sources, speech-language pathologists can better assess, treat, and support adults with communication disorders. As Jessica’s story illustrates, when we address episodic buffer dysfunction directly, we can help individuals transition from fragmented communication to more coherent and satisfying interactions.
The key lies in recognizing that effective communication isn't just about having the right words—it's about having the cognitive infrastructure to weave those words together in a meaningful way. By supporting the episodic buffer through targeted interventions and compensatory strategies, we can help adults with communication disorders reclaim their narrative voices and engage more fully in the social world around them.
As research continues to illuminate the complex relationships between working memory, the episodic buffer, and communication, we're better equipped to provide the comprehensive, evidence-based care that our clients deserve. The future of communication disorder treatment lies not just in addressing symptoms, but in understanding and supporting the underlying cognitive processes that make meaningful communication possible.
The Hidden Link: How Voice Disorders Impact Your Mental Health (And What You Can Do About It)
Discover the surprising link between voice problems and mental health. Learn how voice disorders affect anxiety, depression, and self-esteem, plus practical strategies for recovery through speech therapy and integrated care approaches.
Understanding the Complex Relationship Between Your Voice and Your Mind
When Sarah walked into my speech therapy clinic, she barely whispered her name during our introduction. A successful marketing professional who once led confident presentations, she'd been struggling with vocal strain for months. What surprised her wasn't just the physical discomfort – it was how her voice problems had begun affecting every aspect of her life, from avoiding phone calls to declining social invitations. Sarah's story isn't unique; it highlights a crucial connection that's often overlooked in healthcare: the powerful link between voice disorders and mental health.
Why Your Voice Matters More Than You Think
Your voice is far more than just a tool for communication – it's an extension of your identity, confidence, and emotional well-being. Think about how you feel when you have a bad cold and sound different. Now imagine that feeling persisting for weeks or months with a voice disorder. Research shows that voice problems can create a ripple effect throughout your psychological and social life, impacting everything from self-esteem to career prospects.
Voice disorders affect approximately 10 million people in the United States and Canada, yet the mental health implications often go unaddressed. This oversight represents a significant gap in comprehensive patient care, as studies consistently demonstrate bidirectional relationships between voice problems and psychological well-being.
The Science Behind the Connection
Stress and Anxiety: The Vocal Troublemakers
One of the most compelling areas of research focuses on stress-related voice disorders, particularly vocal cord dysfunction (VCD) or paradoxical vocal fold motion (PVFM). These conditions occur when your vocal cords close inappropriately during breathing, causing symptoms that can mimic asthma.
During the COVID-19 pandemic, researchers documented a remarkable 100% increase in vocal cord dysfunction cases among children – jumping from 5.2% in 2019 to 10.3% in 2020. The common thread? Increased stress and anxiety. Combat veterans also show heightened rates of VCD, with 52% of cases directly linked to high stress and anxiety situations.
The typical patient profile for stress-related voice disorders paints a clear picture: often a high-achieving individual (frequently female) whose symptoms worsen during stressful situations like athletic competitions, important presentations, or emotionally challenging periods. Sound familiar?
The Breathing Connection
Here's where things get interesting from a physiological standpoint. Anxiety directly impacts breathing patterns, and since breath is the foundation of voice production, this creates a perfect storm for voice problems. When you're anxious, you tend to breathe more shallowly and tensely, which can lead to:
Vocal strain and fatigue
Changes in voice quality
Reduced vocal endurance
Increased muscle tension around the larynx
Research in breath-focused voice therapy for females with anxiety shows that addressing breathing patterns can simultaneously improve both voice quality and emotional well-being. Participants reported that as their breathing and voice became more relaxed, their relationship with their voice "evolved to be more centered around compassion, joy, and curiosity".
Beyond Stress: The Broader Mental Health Picture
Self-Esteem and Social Confidence
Voice disorders can create what researchers call a "communicative participation" problem. When your voice doesn't sound the way you expect or want it to, you might start avoiding situations where you need to speak. This avoidance can lead to:
Decreased social interactions
Reduced professional opportunities
Lower self-confidence
Feelings of isolation
Studies show that voice-related quality of life issues are significantly associated with depression and anxiety symptoms. The research indicates that people with voice disorders often experience challenges that extend far beyond the physical symptoms, affecting their overall life satisfaction and mental health.
The Workplace Impact
For professionals whose careers depend on their voice – teachers, salespeople, public speakers, singers – voice disorders can be particularly devastating[8]. The psychological impact often includes:
Career anxiety: Worrying about job performance and security
Identity crisis: Questioning professional competence
Social withdrawal: Avoiding work-related social functions
Increased stress: Creating a vicious cycle that can worsen voice symptoms
The Positive Side: How Voice Therapy Helps Mental Health
Here's the encouraging news: effective voice therapy often provides benefits that extend far beyond improved voice quality. Speech-language pathologists are increasingly recognizing their role in supporting overall well-being, not just communication skills.
Real Results from Real People
Recent research on voice therapy outcomes shows promising mental health benefits. In one study of speech-language pathologist-administered interventions for people with communication disorders, participants showed statistically significant reductions in depression symptoms. While anxiety symptoms also improved, the depression improvements were particularly notable.
A smartphone app study for voice therapy adherence found that when people stuck to their voice therapy programs (which the app helped achieve), they experienced improvements not just in voice quality but in overall quality of life. The key was consistency – those who maintained their therapy routine saw the best outcomes.
The Trauma-Informed Approach
Cutting-edge voice therapy now incorporates trauma-informed care principles, recognizing that many voice disorders, particularly VCD/PVFM, may have psychological components. This approach involves:
Screening for past traumatic experiences
Creating emotionally safe therapy environments
Addressing both physical and emotional aspects of voice disorders
Collaborating with mental health professionals when appropriate
Practical Strategies: What You Can Do Today
For Voice Health and Mental Well-Being
1. Practice Mindful Breathing
Start with just 5 minutes daily of focused breathing exercises. Breathe slowly through your nose, allowing your belly to expand rather than your chest. This simple practice can improve both voice quality and reduce anxiety[1].
2. Stay Hydrated
Proper hydration keeps your vocal cords healthy and flexible. Aim for 8 glasses of water daily, and limit caffeine and alcohol, which can dehydrate your vocal tissues.
3. Manage Stress Proactively
Since stress is such a significant trigger for voice problems, develop healthy coping strategies:
Regular exercise
Adequate sleep (7-9 hours)
Relaxation techniques like meditation or yoga
Time management to reduce overwhelming situations
4. Voice Rest When Needed
If your voice feels strained, give it a break. This doesn't always mean complete silence, but it does mean avoiding shouting, whispering (which can actually strain your voice more), and unnecessary talking.
5. Seek Professional Help Early
Don't wait for voice problems to resolve on their own, especially if they're affecting your daily life or emotional well-being.
When to See a Professional
Consider consulting a speech-language pathologist if you experience:
Hoarseness lasting more than two weeks
Voice changes affecting your work or social life
Breathing difficulties during speaking
Throat pain or strain with voice use
Avoiding speaking situations due to voice concerns
For mental health support, consider counseling if voice problems are causing:
Persistent anxiety about speaking
Depression or mood changes
Social isolation
Significant life disruptions
The Road to Recovery: An Integrated Approach
The most effective treatment for voice disorders with mental health components often involves a team approach. This might include:
Speech-language pathologists for voice therapy and breathing techniques
Mental health counselors for anxiety, depression, or trauma-related issues
Medical doctors for any underlying physical conditions
Occupational therapists for stress management and coping strategies
Sarah, the marketing professional I mentioned earlier, exemplifies this integrated approach. Through voice therapy focused on breathing techniques and stress management, combined with short-term counseling to address her work-related anxiety, she gradually regained both her voice and her confidence. Six months later, she was leading presentations again – and enjoying them.
Looking Forward: Hope and Healing
The connection between voice disorders and mental health is complex, but understanding this relationship opens doors to more effective, compassionate treatment. Your voice is part of who you are, and taking care of it means taking care of your overall well-being.
Remember that voice disorders are highly treatable, and the psychological impacts can improve significantly with proper care. Many people find that addressing their voice problems actually enhances their overall quality of life in unexpected ways, leading to greater confidence, improved relationships, and better stress management skills.
If you're struggling with voice problems, know that you're not alone, and help is available. The journey to vocal health is also a journey to overall wellness – and that's a conversation worth having.
Laryngitis: The Misunderstood Voice Disorder
Your voice suddenly turns hoarse after a loud concert, or you develop an annoying rasp that lingers for weeks. Both may be laryngitis, but they are not the same illness. This friendly guide walks you through why the voice box gets inflamed, how doctors treat it in 2025 and when a raspy voice could signal something more serious.
What Exactly Is Laryngitis?
Laryngitis is inflammation of the larynx—the “voice box” that houses your vocal cords. When those delicate folds swell, they cannot vibrate freely, so your voice sounds hoarse or disappears altogether. Acute laryngitis lasts days to a few weeks, while chronic laryngitis persists for three weeks or longer and often has a different set of triggers.
“I knew something was wrong when the morning announcements came out as a squeak,” recalls Sarah, a fifth-grade teacher who developed acute laryngitis after cheering at a hockey game. Her voice returned in five days—but only after strict vocal rest and plenty of warm tea.
Acute vs. Chronic: A Quick Comparison
Why Does It Strike?
1. Viruses Lead the List
Most acute cases come from the same viral culprits that cause the common cold[2]. The infection irritates the laryngeal lining, similar to how a sunburn irritates skin.
2. Voice Overuse
Shouting at a concert, coaching a team or delivering back-to-back presentations strains the vocal folds. Microscopic tears invite swelling that mimics an infection but is purely mechanical[2].
3. Environmental Irritants
Dry air, cigarette smoke and chemical fumes inflame the mucosa. Long-term exposure can drive chronic hyperplastic laryngitis, a precancerous change seen in factory workers and smokers[4].
4. Gastroesophageal Reflux Disease (GERD) and Silent Reflux (LPR)
When stomach contents reflux into the throat, the acid bathes the larynx, producing chronic irritation, cough and hoarseness[6]. Up to 42 % of reflux patients still have symptoms despite standard once-daily proton-pump inhibitor (PPI) therapy[5].
5. Rare Infectious Agents
Not every chronic case is reflux or smoking related. A traveler in the U.S. developed five years of hoarseness from Mycobacterium kansasii, a non-tuberculous mycobacterium usually found in soil and water[3]. Such cases remind clinicians to biopsy persistent lesions.
6. Historical Curiosities
In 1847, Dr. Horace Green swabbed nitrate of silver directly onto inflamed larynges and reported dramatic relief[1]. The practice is obsolete today, yet it underscores how long we have battled “clergyman’s sore throat.”
Key Symptoms to Watch
Sudden or gradual hoarseness
A “lost” or whisper-like voice
Throat tickle or raw sensation
Dry, barking cough
Trouble projecting or hitting high notes
In chronic cases: globus feeling (a lump in the throat), persistent cough, shortness of breath on exertion[4]
Seek medical care fast if hoarseness lasts longer than three weeks, breathing becomes difficult, or you cough up blood.
Diagnosis: More Than Looking at the Throat
Most acute cases never need a scope; the story alone gives it away. For chronic or atypical cases, ENT specialists may perform:
Flexible laryngoscopy—fiber-optic camera that views the cords while you speak
Stroboscopy—slow-motion view of cord vibration
pH impedance monitoring—detects acid and non-acid reflux when GERD is suspected[6]
Biopsy—rules out dysplasia or cancer in chronic hyperplastic lesions[4]
Modern Treatment Toolbox
Rest & Self-Care
Vocal rest—not complete silence, but using a soft, relaxed voice (not a whisper) for 48–72 hours
Nebulizing with 0.9% saline solution to hydrate and soothe vocal tissues
Drinking water and herbal tea—a simple yet powerful anti-inflammatory
Humidifier for dry indoor air
Medication
Short courses of NSAIDs or corticosteroids for acute swelling (especially singers with a concert looming)
PPIs or H2 blockers for reflux-related laryngitis; dose optimization or twice-daily therapy may be required[5]
Antibiotics only for proven bacterial infections or atypical pathogens such as M. kansasii[3]
Inhaled corticosteroids can ironically cause laryngeal irritation; using a spacer and rinsing reduce this risk.
Voice Therapy
Speech-language pathologists teach healthy phonation, breath support and resonance. Therapy is critical for teachers, coaches and call-center workers who cannot avoid heavy voice use.
When Surgery Enters the Picture
Persistent nodules, polyps or hyperplastic patches may need micro-excision. In a Belarusian series, 47 % of hospitalised chronic hyperplastic laryngitis patients underwent surgical removal of thickened mucosa[4].
Anecdote: The Coach Who Couldn’t Holler
Mark, a 38-year-old basketball coach, pushed through a playoff season with a gravelly voice. Months later he still rasped. Laryngoscopy showed thickened vocal folds and redness. A reflux workup revealed night-time acid exposure. After weight loss, elevating the bed head and split-dose PPIs, his voice cleared within six weeks—proving that sometimes the stomach, not the throat, is the real villain.
Laryngitis vs. Pharyngitis vs. Bronchitis: Spot the Difference
Remember: hoarseness is the hallmark of laryngitis. A painful but clear voice points elsewhere.
Preventing Future Flares
Warm up your voice before public speaking or singing, just as athletes stretch.
Limit caffeine and alcohol that dry mucous membranes.
Quit smoking; smoke is the strongest modifiable risk factor for chronic hyperplastic laryngitis[4].
Manage reflux with small meals, weight control and not lying down within three hours of eating[6].
Use a microphone when teaching large groups—your cords will thank you.
Keep indoor humidity around 40–50 %.
When to Seek Specialist Help
Hoarseness beyond three weeks
Breathing or swallowing difficulty
Neck mass or unexplained weight loss
Systemic symptoms (fever, night sweats)[3]
Recurrent episodes in a professional voice user
Early evaluation not only speeds recovery but can also detect early laryngeal cancer, which often masquerades as “stubborn laryngitis.”
The Take-Home Message
Laryngitis is usually a short-lived nuisance, but it can also be a window into deeper issues—reflux, smoking-related changes, even rare infections. Listen to your voice: if it cries for help longer than a few weeks, let an ENT specialist take a look. Use smart vocal habits, stay hydrated and treat underlying irritants, and your voice will repay you with years of reliable service.
[1] A Treatise on Diseases of the Air-Passages: Comprising an Inquiry into the History, Pathology, Causes, and Treatment of Those Affections of the Throat Called Bronchitis, Chronic Laryngitis, Clergyman's Sore Throat, &c. https://www.semanticscholar.org/paper/1682e99ff884acbdd05f8cd4f1ad0ae9059d2a00[2] Acute laryngitis. Modern aspects of physiotherapy treatment with syndromic and pathogenetic approach https://entru.org/2022-6-114-119.html[3] Chronic laryngitis caused by Mycobacterium Kansasii in a traveler https://onlinelibrary.wiley.com/doi/10.1002/lary.27952[4] Analysis of diagnosis and treatment of chronic hyperplastic laryngitis in Republic of Belarus on example of patients in Dobrush district of Gomel region https://entru.org/2022-4-73-81.html[5] ARE THE PERSISTENT SYMPTOMS TO PROTON PUMP INHIBITOR THERAPY DUE TO REFRACTORY GASTROESOPHAGEAL REFLUX DISEASE OR TO OTHER DISORDERS? http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-28032018000500085&lng=en&tlng=en[6] Extraesophageal manifestations of gastroesophageal reflux disease: cough, asthma, laryngitis, chest pain. https://smw.ch/index.php/smw/article/view/1450
Understanding Aspiration Pneumonia: Causes, Symptoms, and Treatment Options
Aspiration pneumonia occurs when foreign materials are inhaled into the lungs, causing infection and inflammation. This comprehensive guide explores its causes, symptoms, diagnosis methods, treatment approaches, and essential prevention strategies for patients and caregivers.
Aspiration pneumonia remains a significant health concern, particularly among older adults and those with certain risk factors. This comprehensive guide explores what aspiration pneumonia is, how it develops, methods for diagnosis, treatment approaches, and prevention strategies to help patients and caregivers better understand this serious respiratory condition.
What Is Aspiration Pneumonia?
Aspiration pneumonia occurs when foreign materials such as food, liquids, saliva, or stomach contents are inhaled into the lungs rather than being swallowed into the digestive tract. This aspiration causes an infection in the lung tissue, leading to inflammation and potentially serious respiratory complications.
Unlike regular pneumonia, aspiration pneumonia has a distinct cause – the inhalation of foreign substances – but interestingly, there is no universally accepted definition or diagnostic criteria in clinical practice. Medical professionals continue to debate the precise definition, which can complicate diagnosis and treatment.
Consider Mrs. Johnson, an 82-year-old with mild dementia who was hospitalized after family members noticed she was coughing frequently during meals and developed a fever. Her case illustrates a common scenario: aspiration pneumonia often develops gradually in vulnerable individuals as repeated small aspirations damage the lungs over time.
Aspiration Pneumonia vs. Aspiration Pneumonitis
It's important to distinguish between aspiration pneumonia and aspiration pneumonitis, as they require different treatment approaches:
Aspiration pneumonia involves bacterial infection following aspiration of materials containing bacteria, typically from the mouth or stomach.
Aspiration pneumonitis is a chemical injury caused by inhaling sterile gastric contents, resulting in inflammation without initial infection (though secondary infection may develop).
This distinction matters because pneumonitis might not require antibiotics initially, while pneumonia typically does. Research suggests procalcitonin (PCT) levels can help differentiate between these conditions, with normal levels more common in pneumonitis (86.7%) compared to pneumonia (38.8%).
Causes and Risk Factors of Aspiration Pneumonia
Aspiration pneumonia doesn't affect everyone equally. Several risk factors significantly increase vulnerability:
Primary Risk Factors
1. Oropharyngeal dysphagia: Difficulty swallowing significantly raises aspiration risk.
2. Advanced age: Elderly individuals have weakened swallowing reflexes and immune responses.
3. Neurological conditions: Stroke, Parkinson's disease, dementia, and other neurological disorders affect swallowing coordination.
4. Poor oral health: Dental issues increase harmful bacteria in the mouth that can be aspirated.
5. Reduced consciousness: Sedation, anesthesia, or altered mental status from various causes.
Additional Contributing Factors
Recent hospitalization or institutionalization
Use of feeding tubes
Gastroesophageal reflux disease (GERD)
Multiple chronic health conditions (comorbidities)
Weak cough reflex or respiratory muscle weakness
History of previous pneumonia episodes
Think of aspiration risk as a spectrum: we all occasionally aspirate tiny amounts while sleeping, but healthy individuals quickly clear these materials. In contrast, someone like Mr. Thomas, a 75-year-old stroke survivor with swallowing difficulties, faces much higher risks because his protective mechanisms are compromised.
Signs and Symptoms of Aspiration Pneumonia
Recognizing aspiration pneumonia quickly can improve outcomes. Common symptoms include:
Common Symptoms
Fever (though not always present, especially in elderly patients)
Productive cough with discolored sputum
Shortness of breath or increased respiratory rate
Chest pain, particularly with breathing
Fatigue and general weakness
Respiratory distress in severe cases
Associated Signs
Coughing or choking during meals
Gurgling voice after eating or drinking
Changes in breathing patterns
Decreased oxygen saturation levels
Confusion in elderly patients (a common atypical presentation)
Unlike typical community-acquired pneumonia, aspiration pneumonia may develop more gradually. For instance, a nursing home resident might show mild symptoms for days before developing more severe illness, making regular monitoring of at-risk individuals crucial.
Diagnosis: Challenges and Approaches
Diagnosing aspiration pneumonia presents unique challenges due to the lack of standardized criteria. Healthcare providers typically use a combination of approaches:
Clinical Assessment
Medical history review, especially focusing on aspiration risk factors
Physical examination, including lung sounds and vital signs
Observation of swallowing difficulties or reports of choking episodes
Diagnostic Tests
Chest X-ray or CT scan: Looking for infiltrates, typically in dependent lung segments
Blood tests: Complete blood count, inflammatory markers like C-reactive protein (CRP)
Procalcitonin (PCT): Helps distinguish bacterial pneumonia from pneumonitis
Bronchoalveolar lavage (BAL): In certain cases to identify specific bacteria or confirm aspiration
Swallowing assessments: Tests like the repetitive saliva swallowing test (RSST) to evaluate dysphagia risk
Interestingly, recent research suggests we may be overclassifying pneumonia in frail elderly patients as "aspiration pneumonia" based more on patient frailty than on confirmed aspiration events. Some experts suggest using the term "frailty-associated pneumonia" instead. This highlights how diagnosis often relies on presumption of aspiration rather than direct confirmation.
Treatment Options for Aspiration Pneumonia
Treatment approaches for aspiration pneumonia typically involve multiple strategies:
Antibiotic Therapy
The cornerstone of treatment is appropriate antibiotic selection, though specific guidelines vary:
Coverage often targets anaerobic bacteria as well as common respiratory pathogens
Antibiotic choices may include amoxicillin-clavulanate, ampicillin-sulbactam, or clindamycin plus a fluoroquinolone
Treatment duration typically ranges from 5-14 days depending on severity and response
Importantly, not all aspiration episodes require antibiotics. For example, acute aspiration bronchitis without evidence of pneumonia may not benefit from antibiotic treatment for preventing progression to pneumonia.
Supportive Care
Oxygen therapy as needed
Proper positioning to reduce aspiration risk
Adequate hydration and nutrition support
Respiratory therapy and pulmonary hygiene measures
Addressing Underlying Causes
Swallowing rehabilitation with speech therapy
Oral care protocols to reduce harmful bacteria
Treatment of contributing conditions like GERD
Adjusting medications that might affect swallowing
For example, Mrs. Garcia, a 79-year-old with Parkinson's disease, developed aspiration pneumonia after a medication change affected her swallowing. Her treatment included not only antibiotics but also swallowing therapy, medication adjustment, and temporary diet modification – demonstrating the multidisciplinary approach often required.
Prevention Strategies
Prevention is particularly important for aspiration pneumonia, especially given its high recurrence rates. Key strategies include:
For Healthcare Providers
Regular swallowing assessments for at-risk patients
Proper positioning during feeding (sitting upright—not reclined)
Implementation of oral hygiene protocols
Staff training on aspiration risk recognition
Consideration of dysphagia screening tools like RSST
For Caregivers and Patients
Modified food textures and thickened liquids when appropriate
Proper positioning during and after meals
Careful medication administration
Attention to oral hygiene
Recognition of early warning signs
Think of prevention as building multiple barriers against aspiration, similar to how we use multiple safety features in automobiles. Each preventive measure adds another layer of protection for vulnerable individuals.
Special Considerations for Vulnerable Populations
Elderly Patients
The aging population faces particular challenges with aspiration pneumonia:
It's one of the most common types of pneumonia in older adults, with prevalence ranging from 5% to 24% of community-acquired pneumonia admissions
Silent aspiration (aspiration without obvious coughing or choking) is common
Presentations may be atypical, with confusion or general decline rather than respiratory symptoms
Comprehensive approach addressing frailty, nutrition, and overall function is essential
Patients with Dysphagia
For those with swallowing disorders:
Regular swallowing assessments and therapy
Dietary modifications based on individual capabilities
Consideration of feeding alternatives in severe cases
Ongoing rehabilitation to maintain or improve function
Interestingly, research shows that patients admitted with aspiration pneumonia who have a co-diagnosis of dysphagia may actually have lower rates of complications like sepsis, respiratory failure, and mortality – possibly because their risk is recognized and managed proactively.
Prognosis and End-of-Life Considerations
Aspiration pneumonia carries significant mortality risk, especially among frail elderly patients. When discussing prognosis, it's important to consider:
Overall health status and functional level before illness
Response to initial treatments
Presence of complications like respiratory failure or sepsis
Underlying conditions and their severity
For patients with advanced illness or dementia, recurrent aspiration pneumonia may indicate disease progression. This often prompts difficult but necessary conversations about goals of care and quality of life. Some families choose to focus on comfort measures rather than repeated hospitalizations when aspiration pneumonia becomes recurrent in advanced illness.
Conclusion
Aspiration pneumonia represents a significant health challenge that requires a nuanced understanding of its causes, recognition, treatment, and prevention. The approach to this condition continues to evolve, with some experts suggesting we need a paradigm shift in how we conceptualize and manage pneumonia in frail elderly patients.
By recognizing risk factors, implementing preventive strategies, and taking a comprehensive approach to treatment, healthcare providers, patients, and caregivers can work together to reduce the burden of this common but serious condition. The future of aspiration pneumonia management lies in continued research, better diagnostic tools, and integrated care approaches that address the multiple factors contributing to aspiration risk.
Celebrating Speech and Hearing Month 2025: The Power of Communication
May is Speech and Hearing Month! Discover the importance of communication health, how speech therapy transforms lives, and why early intervention matters for speech and language development.
May marks Speech and Hearing Month, a time when speech language pathologists, audiologists, and communication health professionals worldwide celebrate the importance of effective communication. This year is particularly special as 2025 marks the American Speech-Language-Hearing Association's (ASHA) Centennial – 100 years of dedicated service to improving communication health! As speech therapy professionals, we're excited to join this celebration and share why communication matters so much in our everyday lives.
The History Behind Speech and Hearing Month
Did you know that Speech and Hearing Month traces its roots back to 1927? Initially established as National Hearing Week by the Federation of Organizations for the Hard of Hearing, it expanded to Better Hearing Month in 1958 and finally became known as Better Speech and Hearing Month in 1972. For nearly a century, this observance has helped raise awareness about communication disorders and highlighted the vital work of speech-language pathologists and audiologists.
The evolution of this awareness month reflects our growing understanding of communication challenges. What once began as a modest week-long event has blossomed into a month-long campaign that reaches millions. As one audiologist I know likes to say, "We've gone from whispering about speech disorders to having full-volume conversations about them!" That progress alone is worth celebrating.
Why Communication Matters
We often take speaking, hearing, and being understood for granted. However, for those with communication challenges, even simple daily interactions can become difficult hurdles. Communication disorders affect not just the ability to speak or hear but impact physical, emotional, social, and financial well-being.
Consider this: communication touches every aspect of our lives. It's how we:
Connect with loved ones
Succeed professionally
Express our basic needs
Learn and develop
Process our emotions
A parent once told me, "Before speech therapy, my home was filled with frustrated screams. Now it's filled with stories and songs." That transformation – from isolation to connection – illustrates why our work as speech therapists matters so much.
Common Communication Disorders We Treat
Speech Sound Disorders
From the classic lisp (where someone might pronounce "lisp" as "lithp") to rhotacism (difficulty pronouncing the 'r' sound, turning "rabbit" into "wabbit"), speech sound disorders affect clarity and intelligibility. These challenges can range from mild to severe and may persist without proper intervention.
Fluency Disorders
Stuttering affects nearly 80 million people worldwide – about 1% of the population. Despite its portrayal in films like "The King's Speech" (where King George VI worked with speech therapist Lionel Logue to manage his stammer), stuttering remains widely misunderstood. Effective speech therapy approaches can make a tremendous difference for those who stutter.
Language Disorders
Language disorders can affect comprehension, expression, or both. For children, this might mean delayed milestones in babbling or first words[15][17]. For adults who've experienced acquired brain impairment, it might mean relearning language skills after a stroke or injury.
Neurological Speech Disorders
Conditions like dysarthria (where neurological injury affects speech muscles, causing slurred speech) or hypophonia (quiet voice) require specialized therapeutic approaches. Through dedicated speech therapy, many patients experience significant improvements in their ability to communicate.
Developmental Milestones: When Do Babies Start Talking?
Parents often wonder, "When will my baby start talking?" While each child develops at their own pace, certain milestones can help gauge progress:
Birth to 3 months: Smiles, makes cooing sounds, seems to recognize your voice
4 to 6 months: Begins to repeat sounds (like "ba-ba-ba"), responds to sounds
7 to 11 months: Babbles with meaning, may say simple words like "mama" or "dada"
12 to 17 months: Uses 2-3 words meaningfully, follows simple directions
18 to 24 months: Vocabulary expands rapidly, begins forming simple phrases
As one speech-language pathologist in our practice likes to joke, "Babies are like little scientists testing out sounds – except their lab reports come in the form of adorable babbling."
If you notice your child isn't meeting these milestones, don't panic! Early intervention through speech therapy for kids can make a tremendous difference. Remember: early support leads to better outcomes.
The Impact of Speech Therapy: Stories That Inspire
Finding a Voice After Stroke
Last year, we worked with Martin, a retired professor who experienced aphasia following a stroke. Initially unable to form coherent sentences, Martin felt trapped in his own mind. Through dedicated speech and language therapy sessions, he gradually reclaimed his ability to communicate. "Words were always my tools," he told us recently. "Now each recovered word feels like finding a lost treasure."
Overcoming Childhood Apraxia of Speech
Six-year-old Sophia couldn't pronounce her own name when she first came for speech therapy. Her frustrated attempts at communication often ended in tears. After six months of therapeutic speech sessions focusing on motor planning and coordination, Sophia now confidently introduces herself to new friends at school. Her mother reports, "The first time she said 'My name is Sophia' clearly was better than any concert I've ever attended."
Managing Muscle Tension Dysphonia
Professional singer Elena developed muscle tension dysphonia after a respiratory infection. Her voice – her livelihood – became hoarse and unreliable. Working with our speech pathologist and voice clinic specialists, she learned techniques to reduce vocal strain and restore healthy voice production. "It's like my voice went from static to surround sound," Elena explained at her final session.
Our Comprehensive Speech Therapy Services
Our speech therapy practice offers a wide range of services tailored to meet diverse communication needs:
Pediatric speech therapy for developmental speech and language delays
Adult speech rehabilitation following stroke or brain injury
Voice therapy for professionals with vocal demands
Fluency therapy for stuttering and other speech rhythm disorders
Swallowing therapy for dysphagia
Accent modification for clear communication
Group therapy sessions for social communication skills
Whether you're looking for speech therapy in Toronto, speech therapy in Ottawa, Ontario, or virtual services, our team of certified speech-language pathologists can help.
Specialized Approaches for Diverse Needs
Our practice integrates evidence-based approaches including:
PECS (Picture Exchange Communication System) for non-verbal communicators
Speak Out! therapy for Parkinson's speech symptoms
Pivotal response treatment for children with autism
Fine motor coordination activities integrated with speech therapy
S-blends focus for specific articulation challenges
We collaborate with other professionals including audiologists, ENT specialists, and occupational therapists to ensure comprehensive care.
When to Consider Speech Therapy
You might benefit from consulting a speech therapist if:
Your child isn't meeting typical language milestones
You notice signs of echolalia (repeating others' words instead of producing spontaneous speech)[5]
Your child shows persistent patterns like tongue thrust or lisping
You experience voice changes, hoarseness, or loss of voice
Speaking becomes effortful after neurological changes
You have concerns about swallowing safety
Stuttering impacts daily communication
As one client humorously put it, "I knew I needed help when my tongue started feeling like it had its own agenda – and it wasn't following my script!"
Taking the First Step
Communication is too important to leave to chance. If you or someone you love is struggling with speech, language, or hearing challenges, a professional assessment can be the first step toward improvement.
Our team of speech-language pathologists (SLPs) provides compassionate, effective therapy based on the latest research. We believe everyone deserves to be heard and understood.
This Speech and Hearing Month, consider how communication shapes your life – and reach out if you need support. After all, as communication specialists, we're not just good listeners – we're also here to help you find your voice.
Conclusion: Celebrating a Century of Communication Progress
As we celebrate ASHA's centennial during this year's Speech and Hearing Month, we reflect on how far the field of speech-language pathology has come. From the days when stuttering was misunderstood as a psychological quirk to today's neurologically-based treatments, our understanding and approaches have evolved tremendously.
Communication connects us, defines us, and allows us to express our humanity. Whether through spoken words, sign language, or assistive technology, the ability to share our thoughts and feelings remains essential to the human experience.
We're honored to play a role in this important work and look forward to serving our community for years to come. Here's to another century of advancing communication health for all!
Speech Therapy for Parkinson’s Disease: Proven Treatments, Celebrity Stories, and the Road Ahead
Speech and communication challenges are common in Parkinson’s disease, but modern speech therapy offers real hope. From innovative treatments like combining singing with speech exercises to inspiring stories from celebrities with Parkinson’s disease, this post explores proven therapies, new research, and practical tips for improving quality of life at every stage.
Parkinson’s disease (PD) touches millions of lives, from everyday people to world-famous celebrities. If you or a loved one are living with Parkinson’s, you know that the symptoms go far beyond the well-known tremor. Speech and communication challenges are among the most frustrating-and least understood-signs of Parkinson’s disease. But there’s good news: advances in speech therapy are helping people regain their voice, confidence, and social connections.
In this post, we’ll break down the best treatments for Parkinson’s disease speech issues, highlight new research, share stories from celebrities with Parkinson’s disease, and answer your top questions about causes, symptoms, and life with PD.
What Is Parkinson’s Disease?
Parkinson’s disease is a progressive neurological disorder that affects movement, balance, and often speech. The main cause is the loss of dopamine-producing cells in the brain, but the reasons for this loss are still being studied. Genetics, environment, and age all play a role, but for most people, the exact etiology of Parkinson’s disease remains unclear.
Common Symptoms of Parkinson’s Disease
Tremor (shaking, often starting in the hands)
Slowed movement (bradykinesia)
Muscle stiffness
Balance and gait problems
Speech changes (soft voice, monotone, slurred speech)
Masked face (reduced facial expression)
Swallowing difficulties
Parkinson’s disease dementia (in some cases)
Early signs of Parkinson’s disease can be subtle, including changes in handwriting, loss of smell, or a softer voice. If you notice these symptoms, consult a neurologist for proper diagnosis and to discuss treatment options.
Celebrities and Famous People with Parkinson’s Disease
Hearing about celebrities with Parkinson’s disease can be both inspiring and educational. Their openness helps reduce stigma and brings attention to the need for better treatments.
Michael J. Fox: Diagnosed at age 29, Fox has become a global advocate for Parkinson’s research. His foundation has raised over a billion dollars for new treatments for Parkinson’s disease.
Muhammad Ali: The legendary boxer lived with Parkinson’s for decades, raising awareness about the disease’s impact on speech and movement.
Alan Alda: The beloved actor has spoken candidly about his early symptoms of Parkinson’s disease and how he manages them.
Linda Ronstadt: The iconic singer lost her singing voice due to Parkinson’s, highlighting how the disease affects speech and music.
These famous people with Parkinson’s disease remind us that anyone can be affected-and that living well with PD is possible.
Speech Challenges in Parkinson’s Disease
Nearly 90% of people with Parkinson’s disease experience speech and voice problems, known as hypokinetic dysarthria. This can appear at any stage and often worsens as the disease progresses. Symptoms include:
Soft or hoarse voice
Monotone speech
Slurred or mumbled words
Short rushes of speech
Difficulty with swallowing (dysphagia)
These issues can lead to social isolation and frustration, but targeted speech therapy can make a dramatic difference.
Best Treatments for Parkinson’s Disease Speech Problems
1. Intensive Speech Therapy
Research shows that intensive, structured speech therapy is one of the best treatments for Parkinson’s disease speech issues. A recent study found that patients who received speech therapy three times a week for 12 weeks had significant improvements in voice strength, clarity, and overall communication. These gains were still present six months after therapy ended, showing the long-term benefits of sticking with a program4.
Example:
A patient named John, diagnosed with PD at age 62, struggled to be heard in family gatherings. After completing a 12-week intensive speech therapy program, he reported, “I can finally join conversations again. My grandkids don’t ask me to repeat myself anymore!”
2. Combining Speech Therapy with Singing
A new trend in PD treatment is blending conventional speech therapy with singing exercises. In a recent randomized controlled trial, patients who participated in both speech and singing interventions saw greater improvements in voice intensity and quality than those who did only one or the other. Singing helps by engaging respiratory muscles and improving pitch and volume control.
Anecdote:
Linda Ronstadt, whose singing career was cut short by Parkinson’s, has spoken about the emotional impact of losing her voice. While not all patients will sing on stage, singing in therapy can restore confidence and joy in communication.
3. Music Therapy
Music therapy isn’t just for mood-it can directly improve gait and speech in Parkinson’s disease. Studies show that rhythmic cueing and singing exercises can help with both speech clarity and walking stability, especially in advanced stages.
Comparison:
Think of music therapy as a “tune-up” for the brain’s motor circuits. Just as a metronome helps musicians keep time, rhythmic exercises help PD patients coordinate speech and movement.
4. Home-Based and Personalized Speech Therapy
Not everyone can attend frequent clinic visits. The PERSPECTIVE study is testing personalized, home-based speech therapy supported by a training app. Early results suggest this approach can boost speech intelligibility and quality of life, regardless of disease stage.
Example:
Mary, age 70, found it hard to travel to her speech therapy clinic. Using a home-based program with virtual check-ins, she was able to practice daily and saw steady improvement in her speech and confidence.
5. Telerehabilitation and Technology
Smartwatch technology and telehealth platforms are making speech therapy more accessible than ever. Patients can now receive expert guidance and feedback from the comfort of home, which is especially valuable for those with mobility challenges.
Guidelines for Treatment of Parkinson’s Disease Speech Problems
Start Early: Address speech changes as soon as they appear. Early intervention leads to better outcomes.
Be Consistent: Intensive, regular practice is key. Home exercises help maintain gains between sessions.
Personalize Therapy: Work with a speech-language pathologist (SLP) to tailor exercises to your needs and goals.
Include Caregivers: Family support and group therapy can boost motivation and social participation.
New and Emerging Treatments for Parkinson’s Disease
Researchers are always searching for new treatments for Parkinson’s disease, including speech problems. Some promising directions include:
Combining therapies: Integrating music, speech, and movement exercises for a holistic approach.
Wearable tech: Devices that track and prompt speech exercises in real time.
Telehealth expansion: More clinics now offer virtual speech therapy, making expert care available to people everywhere.
Frequently Asked Questions
What are the early signs and symptoms of Parkinson’s disease?
Early signs include tremor, small handwriting, softer voice, and subtle changes in movement or facial expression.
Is Parkinson’s disease hereditary?
Most cases are not directly inherited, but genetics can play a role in some families.
What causes Parkinson’s disease?
The main cause is the loss of dopamine-producing brain cells, but the exact reasons are complex and involve both genetic and environmental factors.
Can Parkinson’s disease be cured?
There is currently no cure, but treatments-including medications, speech therapy, and lifestyle changes-can greatly improve quality of life.
How is Parkinson’s disease diagnosed?
Diagnosis is based on medical history, symptoms, neurological exams, and sometimes brain imaging.
What are the stages of Parkinson’s disease?
PD progresses through stages, from mild symptoms (stage 1) to severe disability (stage 5). Speech problems can appear at any stage.
Is Parkinson’s disease fatal?
PD itself is not directly fatal, but complications (like pneumonia from swallowing problems) can be life-threatening. With good care, many people live for decades after diagnosis.
Can speech therapy help with Parkinson’s disease dementia?
Yes, speech therapy can support communication and swallowing, even when dementia develops.
Real-World Impact: The Power of Speech Therapy
Imagine a support group where everyone speaks softly and hesitantly-until they start group singing as part of their therapy. Within weeks, voices grow stronger, and laughter fills the room. This is the reality for many people with Parkinson’s disease who embrace speech therapy.
Final Thoughts
If you or a loved one are facing Parkinson’s disease, know that you are not alone. From celebrities with Parkinson’s disease who inspire us to the latest research on new treatments, there is hope and help available. Speech therapy-especially when personalized, intensive, and creative-can make a world of difference.
Whether you’re just noticing early symptoms of Parkinson’s disease or navigating advanced stages, don’t hesitate to ask your doctor about speech therapy. The best treatment for Parkinson’s disease is one that’s tailored to you, combining medical care, therapy, and support from family and community.
Stay informed, stay connected, and keep speaking up-your voice matters.
If you’re looking for a speech therapy clinic, speech therapist near you, or want to learn more about guidelines for treatment of Parkinson’s disease, reach out to a certified speech-language pathologist or your local Parkinson’s support organization today.
Vocal Nodules and Polyps: When the Voice Says No
Hoarse voice? Sore throat that just won’t quit? You might be dealing with vocal nodules or polyps. This friendly guide explains what vocal cord nodules are, how to spot symptoms, and what you can do to get your voice back-without losing your sense of humor.
Imagine waking up one morning, ready to kick start your day with your favorite shower tune, only to find your voice sounds more like a rusty hinge than the dulcet tones of Adele. Before you panic and start Googling “Has Julie Andrews sang after her throat surgery?”, let’s talk about what might really be going on with your vocal cords.
What Are Vocal Nodules and Polyps?
Vocal nodules, also known as nodules on vocal cords or vocal fold nodules, are benign (non-cancerous) growths that develop on your vocal cords due to overuse or misuse of your voice. Think of them as the calluses your vocal cords get after too many karaoke nights or shouting at sports games.
Vocal polyps, on the other hand, are like the vocal cord’s version of a blister-often larger and more swollen than nodules, and usually forming on just one side. Both are types of vocal cord lesions, but they have their own quirks.
Quick Comparison Table
Vocal Nodules Symptoms: When to Suspect Your Voice is on Strike
How do you know if you have vocal nodules or a vocal cord polyp? Here are some telltale signs
Hoarseness or a rough, scratchy voice
Breathiness or a weak, airy sound
Voice fatigue (your voice tires out faster than your legs on leg day)
Reduced pitch range (goodbye, Mariah Carey high notes)
Throat pain or soreness, especially after talking or singing
Shooting pain from ear to ear (no, it’s not your headphones)
If you find yourself constantly clearing your throat, or if your friends start offering you tea and honey every time you speak, it might be time to check for vocal nodules symptoms or vocal cord polyp symptoms.
Anecdote: The Case of the Reluctant Rock Star
Let’s take Brenda, a professional singer who noticed her voice getting hoarse after a bout of reflux. Weeks of rest and hydration didn’t help. A visit to her laryngologist confirmed her fears: vocal fold nodules. She learned that nodules aren’t exclusive to screaming rockers; teachers, coaches, and anyone who talks or sings a lot are at risk. Brenda’s story is a reminder that even the most seasoned vocalists need to listen to their bodies (and their voices).
What Causes Vocal Nodules and Polyps?
If you’re wondering why your vocal cords are staging a protest, here are common culprits:
Yelling, screaming, or cheering (e.g. coaches, concern goers)
Singing for long periods without proper technique
Speaking loudly in noisy environments (e.g. teachers, fitness instructors)
Chronic coughing or throat clearing
Smoking or exposure to irritants, including sour-cherry mango vanilla ice vape flavour
Acid reflux (GERD—heartburn or LPR—silent reflux)
Women are statistically more likely to develop vocal nodules, possibly due to anatomical differences and the fact that many voice-heavy professions are female-dominated. So, if you’re a teacher, coach, or singer, your vocal cords might need extra TLC.
Diagnosis: How Do You Know It’s Not Just a Sore Throat?
If your sore throat or persistent hoarseness isn’t going away, it’s time to see a professional. Diagnosing vocal cord nodules, polyps, or other lesions usually involves:
Laryngoscopy: A tiny camera goes on a magical journey through your nose to your throat (don’t worry, it’s not as bad as it sounds).
Stroboscopy: Like a slow-motion replay for your vocal cords, helping doctors see how they vibrate.
Sometimes, a biopsy is needed to rule out anything more serious.
A regular ear nose and throat (ENT) doctor can help, but for voice-specific issues, look for “a laryngologist clinic near me” or “a speech language pathologist near me'“. If you’re in Canada, you can check the public register for certified professionals.
Treatment: How to Get Your Voice Back (aka Defeat Evil Sea Witch Ursula)
Rest, Rest, and More Rest
The first line of defense is vocal rest. That means no singing, yelling, or especially whispering (whispering can be surprisingly harsh on your vocal cords). Think of it as a silent retreat-your vocal cords will thank you.
Voice Therapy: Your Voice’s Personal Trainer
Voice therapy with a speech language pathologist is like sending your vocal cords to the gym, but with less sweat and more humming. Therapy focuses on:
Proper breathing techniques
Gentle vocal exercises
Avoiding vocal abuse (moderating your Guns N’ Roses Karaoke time)
Lifestyle tweaks (hydration, avoiding irritants like smoking)
Surgery: The Last Resort
Most vocal nodules shrink with rest and therapy, but stubborn nodules or polyps might need surgical removal. After surgery, you’ll need more rest and therapy to prevent them from coming back. And yes, you might have a sore throat after surgery, but it’s usually temporary.
Other Treatments
Treating underlying conditions like acid reflux or allergies
Medication for inflammation
Lifestyle changes such as reducing spicy and acidic foods and beverages
Comparisons: Nodules vs. Polyps vs. Other Lesions
What About Surgery for Throat Cancer?
While vocal nodules and polyps are benign, persistent hoarseness can sometimes be a sign of more serious issues like throat cancer. Surgery for throat cancer is a different ballgame, often involving more extensive procedures and longer recovery. If you have risk factors (like smoking) or symptoms that don’t improve, see your ENT promptly.
Frequently Asked Questions
Q: Can I sing again after vocal nodules or surgery?
A: With proper treatment and voice therapy, most people can return to singing or speaking normally. However, it’s important to follow your therapist’s advice to avoid recurrence.
Q: Is a sore throat after surgery normal?
A: Yes, throat pain after surgery is common, but it should improve with time. If your throat hurts after surgery for more than a week or gets worse, contact your doctor.
Q: What’s the difference between a speech pathologist and a speech therapist?
A: They’re the same! Both are trained to help with speech, language, and voice disorders.
How to Find Help: Speech Language Pathologist and ENT Clinic Near Me
If you suspect you have vocal nodules, vocal cord nodules, or a vocal cord lesion, don’t try to diagnose yourself with a mirror and a flashlight (trust us, it won’t end well). Instead:
Search for a speech language pathologist near me or an ENT clinic near me
Check the public register to ensure your provider is certified (CASLPO)
Ask your doctor for a referral
Occupational therapists (OT near me) can also help if your voice issues are affecting your daily life.
Prevention: How to Keep Your Voice Happy
Stay hydrated (water, not coffee or wine-sorry!)
Avoid yelling or speaking over noise
Use amplification when speaking to large groups
Take vocal breaks during long speaking or singing sessions
Treat allergies and acid reflux promptly
Conclusion: Your Voice, You Only Get One
Your voice is one of your most powerful tools-whether you’re a teacher, singer, coach, or professional karaoke enthusiast. Vocal nodules, vocal cord nodules, and polyps can be a setback, but with the right care, treatment, and a little humor, you’ll be back to your old self (or maybe even better).
So, next time you feel a tickle or hoarseness, listen to your body. Give yourself permission to rest, recover, and return to the stage, classroom, or boardroom with confidence.
Why Choose a Speech Pathologist for Communication and Social Skills?
Looking for expert support to boost confidence, improve communication, or help your child thrive socially? Explore how a speech pathologist offers public speaking training near me, child public speaking training near me, and a variety of social skills training near me. Find real-life success stories and compare programs to see how confidence-building classes near me can transform lives for all ages and abilities.
Speech pathologists are uniquely qualified to address not only speech and language challenges but also the broader aspects of communication, confidence, and social interaction. Whether you’re searching for *public speaking training near me* to overcome stage fright, or *social skills training for adults with autism near me* to foster meaningful connections, a speech pathologist can provide personalized, evidence-based support.
A Personal Anecdote: From Hesitant Speaker to Confident Communicator
Consider Sarah, a teenager who struggled with both articulation and anxiety in public speaking. Through individualized sessions with a speech pathologist, she learned techniques to organize her thoughts, use her voice effectively, and manage her nerves. Today, Sarah leads her school’s debate team and mentors younger students-proof that targeted support can unlock hidden potential.
Public Speaking Training Near Me: The Speech Pathologist’s Approach
As a speech pathologist, I offer public speaking training that goes beyond memorizing speeches. My approach focuses on the foundations of effective communication:
Voice projection and clarity
Nonverbal communication and body language
Organizing ideas for clear delivery
Managing anxiety and building confidence
Sessions are tailored for all ages, from school-aged children to adults, and can be offered individually or in small groups.
Example:
A local high school student, initially terrified of presentations, gained the skills and self-assurance to deliver a compelling speech at graduation after just a few months of training.
Child Public Speaking Training Near Me
Early intervention is key for children who are shy, have articulation challenges, or simply want to build leadership skills. As a speech pathologist, I use playful, engaging activities to help children:
Practice public speaking in a safe, supportive environment
Develop clear speech and expressive language
Gain confidence through positive reinforcement
Anecdote:
A seven-year-old client, once too nervous to speak in class, now eagerly volunteers to read aloud and has even participated in a local storytelling contest.
Confidence Building Classes Near Me
Confidence is at the heart of all successful communication. My confidence building classes, grounded in speech-language pathology, teach practical strategies such as:
Positive self-talk and mindset shifts
Relaxation and breathing techniques
Gradual exposure to challenging situations
Social Skills Training Near Me: For All Ages and Needs
Speech pathologists are experts in social communication. Whether you’re seeking *social skills training groups near me* or *social skills training for adults with social anxiety near me*, I offer programs that address:
Initiating and maintaining conversations
Understanding nonverbal cues
Navigating group dynamics
Building and maintaining friendships
For Children: Social Skills Training for Kids Near Me
Sessions use games, role-playing, and group activities to help children practice and generalize social skills in real-life settings.
Anecdote:
A child with ADHD who struggled to make friends learned to take turns, listen actively, and join group play-leading to more positive peer relationships.
For Adults: Social Skills Training for Adults Near Me
Adults may face challenges due to social anxiety, autism, or simply lack of experience. My sessions provide a safe space to:
Practice conversational skills
Build confidence in social situations
Learn strategies for managing anxiety
Example:
A client with social anxiety reported feeling comfortable at networking events for the first time after participating in a targeted social skills group.
Specialized Social Skills Training
Social Skills Training for Adults with Autism Near Me
Adults with autism often benefit from explicit instruction in social norms, relationship-building, and emotional regulation. My programs use evidence-based techniques, including video modeling and social narratives, to support meaningful progress.
ADHD Social Skills Training Near Me
For individuals with ADHD, I focus on impulse control, listening skills, and reading social cues through structured activities and real-time feedback.
Social Skills Training for Adults with Social Anxiety Near Me
Gradual exposure and cognitive-behavioral strategies help adults with social anxiety gain confidence and reduce avoidance behaviors.
Autism Social Skills Training Near Me
For children and teens with autism, I offer both individual and group sessions, focusing on communication, play skills, and emotional understanding.
Social Skills Training Groups Near Me: The Value of Group Practice
Group-based sessions allow participants to learn from each other, practice new skills in a supportive setting, and receive immediate feedback from a speech pathologist. Whether you’re looking for *social skill training near me* for your child or yourself, group programs foster community and accountability.
How to Choose the Right Speech Pathologist
When searching for *public speaking training near me* or *social skills training autism near me*, consider these tips:
Credentials: Ensure your provider is a certified speech-language pathologist (SLP).
Experience: Look for expertise with your specific age group or diagnosis (e.g., autism, ADHD).
Approach: Ask about individualized plans and evidence-based methods.
Success Stories: Request references or testimonials from past clients.
Real-Life Success: Investing In Confidence
Across all ages, clients who invest in speech pathology services report dramatic improvements in confidence, communication, and social connection. From the child who finds their voice in a school play, to the adult who overcomes social anxiety and builds new friendships, the results speak for themselves.
Conclusion: Your Path to Confident Communication Starts Here
Whether you’re searching for *public speaking training near me*, *child public speaking training near me*, or *confidence building classes near me*, working with a speech pathologist offers expert guidance tailored to your unique needs. Take the first step-invest with confidence in yourself or your child, and unlock a future filled with opportunity and connection.
Throat Cancer: Recognizing the Signs That Shouldn't Be Ignored
A persistent sore throat might be more than just a cold. Discover the critical signs of throat cancer, risk factors like HPV, and how early detection dramatically improves outcomes.
Persistent sore throat that just won't quit? While most throat discomfort stems from harmless causes, knowing when to be concerned could literally save your life. As someone who's researched extensively into this topic, I've created this comprehensive guide to help you understand throat cancer symptoms, risk factors, and when that nagging throat pain deserves medical attention.
Understanding Throat Cancer: The Basics
Throat cancer refers to cancerous growths that develop in your throat (pharynx), voice box (larynx), or tonsils. Think of your throat as Grand Central Station for breathing, speaking, and eating – when cancer disrupts this busy terminal, multiple bodily functions can be affected.
"What is throat cancer exactly?" my friend John asked after his diagnosis. I explained that throat cancer occurs when cells in the throat develop genetic mutations, causing them to grow uncontrollably and potentially spread. Like unwanted guests who arrive, make themselves at home, and invite friends, these cancer cells disrupt normal throat function as they multiply.
Different types of throat cancer exist, with squamous cell throat cancer being the most common, accounting for about 90% of cases. Other types include adenocarcinoma, lymphoma in the throat area, and more rarely, sarcoma. Each type may present slightly differently and require specific treatment approaches.
Early Warning Signs: What Does Throat Cancer Feel Like?
Early signs of throat cancer can be subtle and easily mistaken for common ailments like colds or allergies. However, persistence is the key differentiator – throat cancer symptoms typically don't resolve with time or standard treatments.
Common Early Symptoms Include:
Persistent sore throat (especially a sore throat for 3 weeks or longer)
Constant throat clearing (that constant throat clearing cancer patients often describe as their first symptom)
Hoarseness or voice changes lasting more than two weeks
Difficulty swallowing (dysphagia)
Feeling like something is stuck in your throat (even when you're not eating)
Ear pain (particularly on one side)
Unexplained weight loss
Swollen lymph nodes in the neck
One throat cancer survivor described her early symptoms this way: "It felt like I had swallowed a small fish bone that wouldn't go away no matter how much water I drank.” That persistent tickle that throat cancer patients often describe was the first clue something wasn't right.
Visual Symptoms: What Does Throat Cancer Look Like?
If you're wondering what throat cancer looks like, visual symptoms can include:
Red patches in the throat
White patches (leukoplakia)
Unusual growths or lumps
Swelling in one area of the throat
Asymmetry of throat tissues
Early stage white spots throat cancer may present can resemble a strep infection or oral thrush, making self-diagnosis challenging. That's why throat cancer pictures from medical sources can be helpful for awareness, though they shouldn't replace professional evaluation.
First signs of throat cancer pictures typically show subtle changes that might not alarm the average person. Cancer back of throat is particularly difficult to visualize without special equipment, which is why unusual sensations deserve attention even when you can't see anything unusual yourself.
The HPV Connection: A Growing Concern
Human papillomavirus (HPV) and throat cancer have a significant connection that's changed our understanding of who gets this disease. HPV throat cancer has been increasing, particularly affecting adults in their 40s and 50s who don't have traditional risk factors like smoking.
"I never smoked a day in my life," shared Michael, a 48-year-old teacher diagnosed with HPV-related throat cancer. "My doctor explained that HPV throat cancer symptoms can be identical to non-HPV cases, but they often respond better to treatment."
Actor Michael Douglas notably brought attention to this connection when he discussed his own experience with HPV throat cancer. The good news? HPV throat cancer generally has better survival rates than tobacco-related cases, with many patients achieving complete remission.
For those wondering how likely is it to get throat cancer from HPV, the risk is relatively low considering how common HPV infection is. Most people clear the virus naturally, but persistent high-risk HPV infections can sometimes lead to cancer years or even decades later.
Risk Factors: What Causes Throat Cancer?
Understanding throat cancer causes can help identify those at higher risk:
1. Tobacco use (smoking, chewing tobacco, or snuff)
2. Heavy alcohol consumption (especially when combined with tobacco)
3. HPV infection (particularly HPV-16)
4. Poor oral hygiene
5. Gastroesophageal reflux disease (GERD) – acid reflux throat cancer risk increases with chronic irritation
6. Family history of cancer
7. Exposure to certain workplace chemicals
Just as sun exposure gradually damages skin, years of exposing throat tissues to irritants like tobacco smoke or alcohol can cause cellular changes. It's like repeatedly scratching the same spot on your arm – eventually, the skin changes in response to the constant irritation.
At-Home Awareness: When to Be Concerned
While there's no definitive way how to check for throat cancer at home, being aware of persistent symptoms is crucial. Compare it to knowing your car – you might not be a mechanic, but you recognize when something sounds or feels off and needs professional attention.
"I kept asking Dr. Google how to know if I have throat cancer instead of seeing an actual doctor," admits Sara, who eventually received an early-stage diagnosis. "Looking back, I wasted precious months trying to self-diagnose when I should have sought medical help for my persistent symptoms."
If you're wondering how to tell if you have throat cancer, ask yourself these questions:
Have my symptoms persisted for more than three weeks?
Are over-the-counter treatments failing to provide relief?
Am I experiencing pain, difficulty swallowing, or voice changes?
Have I noticed any lumps in my neck?
Does my throat look different when I examine it with a flashlight?
Affirmative answers warrant a medical consultation. Remember, early detection dramatically improves outcomes.
Diagnosis Process: What to Expect
If throat cancer is suspected, your doctor may:
1. Perform a thorough examination of your mouth, throat, and neck
2. Use an endoscope (a thin, flexible tube with a light) to examine deeper throat areas
3. Recommend imaging tests like CT scans, MRIs, or PET scans
4. Take a biopsy (tissue sample) of any suspicious areas
The diagnosis process might feel like being a detective's subject – lots of questions, examinations, and tests. But this thoroughness is crucial for accurate diagnosis and appropriate treatment planning.
Treatment Options and Survival Outlook
Is throat cancer curable? Often, yes – especially when caught early. Is throat cancer treatable? Absolutely, even in advanced stages, though treatment becomes more complex.
Treatment approaches may include:
Surgery to remove cancerous tissue
Radiation therapy
Chemotherapy
Targeted therapy
Immunotherapy
A combination of these approaches
Throat cancer survival rate varies significantly based on stage at diagnosis, location, and other factors. The 5-year survival rate ranges from above 80% for early-stage cancers to around 30-40% for stage 4 throat cancer. However, these are statistics, not guarantees – many patients outlive the averages.
"When I was diagnosed with neck and throat cancer, my doctor explained treatment as a 'full-court press' approach," explains Robert, a 5-year survivor. "Different specialists worked together like a well-coordinated sports team to attack the cancer from multiple angles."
Special Considerations for Women
Woman throat cancer symptoms can sometimes be overlooked or attributed to other conditions, as women historically have lower rates of throat cancer than men. However, rates in women are increasing, particularly HPV-related cases.
"My doctor initially thought my hoarseness was related to thyroid issues common in women my age," shares Elaine, diagnosed at 52. "Women need to be especially assertive about persistent throat symptoms, as we're not the 'typical' patient doctors might be looking for."
Personal Stories: How I Knew I Had Throat Cancer
Personal accounts often highlight the subtle progression of symptoms:
"It started with what I thought was seasonal allergies," recalls James. "Then my voice became raspy, like I was doing a bad Batman impression all the time. By the time I developed pain when swallowing hot liquids, the cancer had already progressed more than I'd realized."
Another survivor described her experience: "For months, I had this annoying sensation of needing to clear my throat constantly. It was like having a permanent crumb stuck in there – irritating but not painful enough to seem serious. That constant throat clearing was actually an early warning sign."
Prevention and Screening
While there's no standard screening test for throat cancer, prevention strategies include:
1. Avoiding tobacco products
2. Limiting alcohol consumption
3. Getting vaccinated against HPV (ideally before sexual activity begins)
4. Practicing good oral hygiene
5. Getting regular dental check-ups (dentists often examine the throat)
6. Eating a diet rich in fruits and vegetables
7. Addressing chronic acid reflux
Think of these preventive measures as installing a security system for your body – they don't guarantee you'll never have a problem, but they significantly reduce your risk.
When to See a Doctor
Don't wait to seek medical attention if you experience:
A sore throat lasting more than three weeks
Persistent hoarseness or voice changes
A lump in your neck (throat cancer lump in neck is often how the disease is first detected)
Difficulty or pain when swallowing
Unexplained weight loss
Ear pain without ear infection
As one of my ENT colleaguse likes to say, "A three-week rule applies to most throat symptoms – if it hasn't improved in three weeks, it's time for professional evaluation."
Finding Hope in Early Detection
Remember, most persistent throat symptoms aren't cancer, but they still deserve attention. A friend recently panicked about a persistent sore throat only to discover it was from undiagnosed allergies – but her proactive approach meant she didn't waste time wondering if it was something worse.
When it comes to throat cancer symptoms, knowledge truly is power. By understanding the warning signs and seeking timely medical attention, you're taking control of your health. After all, your throat works hard for you every day – speaking, swallowing, breathing – so return the favor by listening when it tries to tell you something's wrong.
Think of it this way: We'd never ignore a car that makes strange noises for weeks on end, yet we sometimes dismiss our body's warning signals. Be as attentive to your health as you would be to that check engine light – your life may depend on it.
How to Cure Eustachian Tube Dysfunction: A Complete Guide to Relief
After struggling with eustachian tube dysfunction for years, I finally found relief through a combination of medical treatments and natural remedies. Here's everything you need to know about ETD symptoms, causes, and the most effective treatments available today.
Are you tired of that constant ear fullness, popping, or muffled hearing? You're not alone on this journey. Many of my clients suffer with this condition and I’ve collected a wealth of information about treating this annoying affliction.
Understanding Eustachian Tube Dysfunction
Picture this: You’re sitting on an airplane, descending into Denver, when suddenly your ears refuse to pop despite all your yawning, swallowing, and desperate jaw movements. The pressure builds, pain intensifies, and by the time we land, you can barely hear the flight attendant's announcements. Little did you know, this wasn't just a typical case of airplane ears—it was an introduction to eustachian tube dysfunction.
What is eustachian tube dysfunction exactly? Your eustachian tubes are narrow channels that connect your middle ears to the back of your throat. These tiny biological marvels perform a crucial job: equalizing pressure between your middle ear and the outside world (similar to how a submarine uses valves to manage pressure underwater). When functioning properly, these tubes open when you yawn, swallow, or chew, allowing air to flow in and out of your middle ear. However, when dysfunction occurs, this equalization process fails, creating uncomfortable and sometimes painful symptoms.
Eustachian Tube Dysfunction Symptoms
Recognizing the symptoms of eustachian tube dysfunction was my first step toward healing. Perhaps you'll recognize some of these in your own experience:
A persistent feeling of fullness or pressure in your ears (like wearing invisible earplugs)
Muffled hearing that makes everyone sound like they're talking through a pillow
Popping, clicking, or crackling sounds when you swallow or yawn
Tinnitus (that lovely ringing or buzzing that becomes your unwanted companion)
Ear pain ranging from mild discomfort to sharp, stabbing sensations
Dizziness or problems with balance, making you look like you've had one too many drinks
A sensation that your own voice sounds unusually loud inside your head
For many, the muffled hearing was the worst. You may find yourself constantly asking friends to repeat themselves, eventually avoiding social gatherings altogether. Can eustachian tube dysfunction cause fatigue? Absolutely! The constant strain of trying to hear properly, coupled with disrupted sleep from ear discomfort, can be exhausting.
What Causes Eustachian Tube Dysfunction?
Understanding eustachian tube dysfunction causes:
1. Upper respiratory infections (that cold that just won't quit)
2. Allergies (seasonal nemesis)
3. Sinus infections (the unwelcome houseguest)
4. Changes in altitude (flying, diving, or mountain climbing)
5. Enlarged adenoids, especially in children
6. Smoking or exposure to secondhand smoke
7. Obesity, which can cause increased pressure on the tubes
8. TMJ and eustachian tube dysfunction often go hand in hand due to their close anatomical relationship
For many, it turns out to be a combination of seasonal allergies and frequent air travel. It's like your ears are caught in the perfect storm! Does eustachian tube dysfunction go away on its own? Sometimes it does, especially if it's related to a temporary condition like a cold. However, chronic eustachian tube dysfunction requires more deliberate intervention.
Types of Eustachian Tube Dysfunction
Not all ear pressure problems are created equal. Doctors recognize different types of this condition:
Obstructive Eustachian Tube Dysfunction
This most common type occurs when your tubes can't open properly due to inflammation or blockage. It feels like your ears need to pop, but stubbornly refuse to do so. For many sufferers, the issue was primarily with obstructive eustachian tube dysfunction, which felt like having permanently clogged ears.
Patulous Eustachian Tube Dysfunction
Patulous eustachian tube dysfunction is the rebellious cousin of the condition. Instead of staying closed when they should, the tubes remain abnormally open. This creates bizarre sensations like hearing your own breathing or voice unusually loudly (autophony). Imagine having a built-in microphone amplifying your internal sounds—not exactly a superpower anyone wants!
Bilateral vs. Unilateral ETD
You might experience dysfunction of both eustachian tubes (bilateral) or just in one ear (left eustachian tube dysfunction or right eustachian tube dysfunction). Bilateral eustachian tube dysfunction could be your particular joy—double the trouble, double the fun!
Getting a Diagnosis
After months of suffering, most will finally seek medical help. ENTs usually perform several tests, including a tympanometry to measure ear pressure and eardrum movement. For medical coding purposes, you might see eustachian tube dysfunction ICD 10 code H69.90 on your paperwork, or more specifically:
Dysfunction of eustachian tube ICD 10: H69.9
Dysfunctional eustachian tube ICD 10: H69.9
Bilateral eustachian tube dysfunction ICD 10: H69.93
For one-sided issues: dysfunction of right eustachian tube or dysfunction of left eustachian tube
That clinical language might seem dry, but those codes help ensure your insurance properly covers treatment. It's like having the secret password to the healthcare system!
Eustachian Tube Dysfunction Treatment Options
Treating eustachian tube dysfunction can became a mission. Here’s a list of what works best:
Medical Treatments
Your doctor will usually first recommend conservative approaches:
1. Nasal Steroids: Flonase for eustachian tube dysfunction. By reducing nasal inflammation, flonase and eustachian tube dysfunction became less of an issue. You can spray each morning and evening, and within a week, many notice significant improvement.
2. Antihistamines: For allergy-related ETD, the best antihistamine for eustachian tube dysfunction depends on your specific triggers. Non-drowsy options like cetirizine worked well for my daytime symptoms.
3. Decongestants: Is Sudafed good for eustachian tube dysfunction? For many, absolutely! The best decongestant for eustachian tube dysfunction during acute flare-ups was pseudoephedrine, though it's not recommended for long-term use.
4. Antibiotics: Sometimes prescribed if bacterial infection is the suspected cause.
Eustachian Tube Dysfunction Surgery
For persistent cases, eustachian tube dysfunction surgery might be recommended:
1. Myringotomy: A tiny incision in the eardrum to relieve pressure and drain fluid.
2. Tubes for Eustachian Tube Dysfunction: Eustachian tube dysfunction tubes (also called pressure equalization tubes or PE tubes) can be inserted through the eardrum to help with pressure regulation. The eustachian tube dysfunction procedure is relatively quick, performed in-office in many cases.
3. Balloon Dilation: An emerging eustachian tube dysfunction operation where a small balloon is inserted and inflated to expand the tube. Think of it as angioplasty, but for your ears!
Most people can ultimately avoid eustachian tube dysfunction surgery by finding relief through less invasive methods, but it's good to know these options exist for severe cases.
Eustachian Tube Dysfunction Remedies at Home
How to fix eustachian tube dysfunction without medical interventions? Here are several effective eustachian tube dysfunction treatment at home options:
1. Steam Inhalation: Sitting in a steamy bathroom for 15 minutes daily helped open my tubes naturally. It's like creating your personal ear sauna!
2. Nasal Irrigation: Using a neti pot with sterile saline solution cleared my nasal passages and reduced inflammation. Yes, it looks and feels strange but the relief is worth it. Always use sterile water, never tap water.
3. Hydration: Drinking plenty of water thins mucus and helps your eustachian tubes function better. Carry a water bottle everywhere like you’re Gollum and it’s your precioussss.
4. Vitamins for Eustachian Tube Dysfunction: Vitamin A for eustachian tube dysfunction supports healthy mucous membranes. Vitamin A and eustachian tube dysfunction studies suggest it may help maintain proper tube function. Careful not to exceed recommended daily limits.
5. The Best Nasal Spray for Eustachian Tube Dysfunction: For many, a simple saline spray used several times daily kept my nasal passages moist and reduced inflammation.
Eustachian Tube Dysfunction Exercises
Learning how to treat eustachian tube dysfunction through specific movements is revolutionary. These eustachian tube dysfunction exercises are good to use on the go or whenever needed:
1. The Toynbee Maneuver: Pinch your nose closed while swallowing. This creates negative pressure that can help open the tubes.
2. The Valsalva Maneuver: Pinch your nose closed, close your mouth, and gently blow as if trying to pop your ears. Don’t use this technique if you have heart disease.
3. Jaw Exercises: Simple movements like yawning, chewing gum, or moving your jaw side to side can help activate the muscles around your eustachian tubes.
How I Cured My Eustachian Tube Dysfunction Naturally
For most, eustachian tube dysfunction cures come through a comprehensive approach. How long does eustachian tube dysfunction last? Without intervention, it can persist for months or even become chronic. But here's how you may find relief:
1. Identifying Triggers: keep a detailed journal tracking when symptoms worsened and discover patterns related to certain foods, weather changes, and stress.
2. Elimination Diet: Removing dairy and gluten can dramatically reduce symptoms. Apparently, ears have dietary preferences we weren't aware of!
3. Regular Exercise: Moderate daily activity improved circulation and seems to help with ear pressure. Morning jogs become ear therapy sessions.
4. Stress Management: Meditation and deep breathing exercises reduced overall inflammation the body. Ears apparently appreciate zen moments as much as the mind does.
5. Consistent Application: The key to curing eustachian tube dysfunction naturally is consistency. Treat your regimen like a part-time job, never skipping a day.
Within about three months of this comprehensive approach, symptoms should improve. Is it a complete cure for eustachian tube dysfunction? Perhaps not, but it can provide life-changing relief.
Living with Eustachian Tube Dysfunction
For those wondering how long can eustachian tube dysfunction last, the answer varies. For some, it's a temporary inconvenience following a cold. For others with chronic eustachian tube dysfunction, it becomes a condition to manage rather than cure completely.
Flying with Eustachian Tube Dysfunction
Traveling creates special challenges. Here are several tricks for flying with eustachian tube dysfunction:
1. Use a decongestant 30 minutes before takeoff and landing
2. Stay hydrated throughout the flight (avoid alcohol and caffeine)
3. Use special earplugs designed for air pressure regulation
4. Perform the Valsalva maneuver gently during descent (talk to doctor if you have heart disease)
These strategies can transform flying from a painful ordeal to a manageable experience. No more arriving at destinations feeling like your head is underwater!
Eustachian Tube Dysfunction and Tinnitus
The relationship between eustachian tube dysfunction and tinnitus is particularly challenging. Can eustachian tube dysfunction cause tinnitus? Absolutely. The pressure changes and middle ear problems can trigger or worsen that infamous ringing or buzzing.
For many, as their ETD improved, so did their tinnitus.
Can Eustachian Tube Dysfunction Cause Dizziness?
Does eustachian tube dysfunction cause dizziness? For many, yes. Eustachian tube dysfunction dizziness occurs because your inner ear helps maintain balance, and pressure abnormalities can disrupt this system. During severe flare-ups, some may feel feel like they are walking on a rocking boat. Eustachian tube dysfunction and vertigo can be related in some cases, though true vertigo usually involves a spinning sensation that most with ETD fortunately don’t experience.
Other Interesting Connections
Atypical connections to ETD:
TMJ and Eustachian Tube Dysfunction
The temporomandibular joint (jaw joint) sits very close to the eustachian tubes. TMJ eustachian tube dysfunction connections are well-documented, as inflammation or misalignment in the jaw can directly impact ear function. Dentists often spot signs of nighttime teeth grinding which can contribute to ear problems!
Can a Tooth Infection Cause Eustachian Tube Dysfunction?
Surprisingly, yes! The proximity of dental roots to the sinuses means that infection can spread and affect the eustachian tubes. While this isn’t a common cause, it highlights how interconnected our ear health is with other systems.
Eustachian Tube Dysfunction Reddit Communities
For many, valuable resources can be found in online communities. Eustachian tube dysfunction Reddit groups provided support, treatment ideas, and validation when it feels like you are the only one experiencing these strange symptoms. There's something incredibly comforting about finding your "ear people" who truly understand what you're going through.
Is Eustachian Tube Dysfunction Permanent?
The question everyone wants answered: is eustachian tube dysfunction permanent? Based on both research and clinical experience, I can say that while some cases may be chronic, most can be significantly improved or resolved with proper treatment and lifestyle modifications.
Can eustachian tube dysfunction be cured completely? For many people, yes. For others, it becomes a manageable condition with occasional flare-ups. The key is finding your personal treatment formula—the unique combination of medical interventions, lifestyle changes, and self-care practices that work for your specific situation.
Final Thoughts: There Is Hope
If you're currently in the midst of your own eustachian tube dysfunction journey, I want to leave you with a message of hope. The constant ear pressure, muffled hearing, and annoying symptoms may feel overwhelming now, but with persistence and the right approach, relief is possible.
Remember that eustachian tube dysfunction management is often about finding what works for your unique body and situation. What works for some might need adaptation for you, but the framework—identifying causes, trying various treatments systematically, and maintaining consistency—applies universally.
Don't give up if the first few treatments don't provide relief. One’s journey to cure eustachian tube dysfunction takes patience, but the reward of being able to hear clearly, fly comfortably, and live without constant ear pressure is worth every effort.
Have you found particular treatments or approaches that helped your ETD? Or are you just beginning your journey to relief? Either way, you're not alone, and better ear days are ahead!
The Complete Guide to Advocating for Yourself: Master Assertive Communication and Healthy Boundaries
Self-advocacy is a vital life skill that empowers you to stand up for your needs and values. Learn how to communicate assertively and establish healthy boundaries with this comprehensive, easy-to-follow guide
Finding your voice and standing up for your needs is a journey many of us struggle with. Whether you're overwhelmed with requests at work or feeling drained in personal relationships, learning self-advocacy can transform how you navigate life's challenges. This guide explores how to communicate assertively and establish healthy boundaries—essential skills that help you honor your needs while maintaining positive relationships.
Understanding Self-Advocacy: Your Right to Express Your Needs
Self-advocacy meaning goes beyond simply speaking up—it's about recognizing your worth and believing your needs matter. At its core, the self advocacy definition encompasses the ability to understand what you need and effectively communicate those needs to others.
"Before I learned to advocate for myself, I was constantly exhausted and resentful," shares Maria, a marketing professional. "I thought saying yes to everything made me a good team player, but it actually made me less effective at my job and unhappy at home."
What Does It Mean to Advocate for Yourself?
To define self advocacy properly, we need to recognize it as a skill that combines self-awareness, clear communication, and the courage to express your needs. When you advocate for yourself, you:
Identify your own needs and limitations
Express those needs clearly to others
Stand firm when faced with resistance
Negotiate for fair treatment
Protect your well-being through boundary-setting
Think of advocacy for yourself like being your own best friend. Would you let someone treat your best friend unfairly? Probably not! Yet we often accept treatment for ourselves that we'd never allow for someone we care about. Learning to self advocate meaning you extend that same protection to yourself.
Why Self-Advocacy Matters in Every Area of Life
The ability to advocate for yourself impacts everything from career advancement to personal relationships. In the workplace, those who can advocate for themselves are more likely to receive fair compensation, reasonable workloads, and appropriate recognition for their contributions. In personal relationships, self-advocacy prevents resentment and fosters authentic connections based on mutual respect.
Compare someone who struggles with self-advocacy to a smartphone with a dying battery that never gets plugged in—eventually, they'll shut down! Just as your phone needs recharging, your well-being requires you to speak up for your needs.
Assertive Communication: The Foundation of Self-Advocacy
Understanding assertive communication definition is essential for effective self-advocacy. Assertive communication sits in the sweet spot between passive and aggressive styles—it's respectful yet firm, clear yet kind.
What Makes Someone an Assertive Communicator?
An assertive communicator expresses their thoughts, feelings, and needs directly while still respecting others. The assertive communication meaning involves standing up for yourself without stepping on others.
To explain assertive communication more clearly, let's look at how different communication styles might handle the same situation:
Assertive Communication Examples in Action
Imagine your colleague repeatedly interrupts you during team meetings:
Passive response: Say nothing and fume silently, eventually avoiding sharing ideas altogether.
Aggressive response: "Will you shut up and let me finish for once?!"
Assertive response:"I'd like to finish my thought before moving on. When I'm interrupted, I lose my train of thought, and I believe my complete idea would be valuable to the team."
The assertive example communicates the need clearly while maintaining respect—that's the essence of communicate assertively definition.
Key Assertive Communication Skills to Develop
What is an assertive communicator's toolkit? Here are essential skills that define assertive communication:
1. Using "I" statements - "I feel frustrated when..." rather than "You always make me feel..."
2. Maintaining appropriate eye contact - Not staring aggressively or looking away submissively
3. Speaking with a calm, steady voice - Neither shouting nor mumbling
4. Expressing needs directly - Stating what you want rather than hinting
5. Listening respectfully - Showing others the same consideration you expect
"Becoming assertive was like finding the volume control on my communication," jokes Tim, a teacher who struggled with classroom management. "Before, I was either on mute or full blast—neither worked well!"
The Assertive Communication Style Across Situations
Assertive communication style adapts to different contexts while maintaining its core principles. For example:
At work: "I'll need an extension on this deadline to deliver quality work. Can we discuss a more realistic timeline?"
With friends: "I appreciate the invitation, but I need a quiet evening at home tonight."
In relationships: "When household chores aren't shared, I feel overwhelmed and resentful. I'd like us to create a more balanced system."
These assertive examples demonstrate how to express needs clearly while maintaining respect—hallmarks of assertive behaviour.
Understanding Boundaries: Your Personal Protection System
To fully embrace self-advocacy, you need to define boundaries in your life. But what exactly are they? Boundaries meaning, at its simplest, is knowing where you end and others begin.
Boundaries Definition: Your Personal Rulebook
Think of boundaries as your personal instruction manual that teaches others how to treat you. The boundaries definition includes the limits and rules that define what you find acceptable and unacceptable in your interactions with others.
What is the boundary between healthy giving and self-sacrifice? Between helpful feedback and hurtful criticism? Between closeness and invasion of privacy? Only you can define these lines for yourself.
Why Healthy Boundaries Matter
Healthy boundaries are like the walls of your home—they keep the good stuff in and the unwanted elements out. Without them, anyone can wander in and take whatever they want, leaving you feeling violated and depleted.
"I used to think having no boundaries made me generous," shares Jamal, a social worker. "But I realized it actually made me resentful. Setting boundaries allows me to give from a place of fullness rather than emptiness."
How to Create Boundaries in Different Areas of Life
Learning how to build boundaries is a process that requires practice and persistence. Let's explore how to develop boundaries in various contexts:
Setting Personal Boundaries: Your Non-Negotiables
Personal boundaries reflect your core values and needs. These might include:
How much alone time you need
Your comfort level with physical touch
How you prefer to be spoken to
Your privacy requirements
Your financial independence
To establish these, start by identifying your deal-breakers—those lines that, when crossed, leave you feeling uncomfortable or resentful.
Setting Boundaries in Relationships: Creating Healthy Partnerships
Relationship boundaries help both partners thrive while maintaining their individuality. Healthy relationship boundaries might include:
Respecting each other's need for separate friendships and interests
Agreeing on how to handle finances
Defining comfortable levels of intimacy
Determining how much time to spend together versus apart
Establishing communication expectations
"Before learning about boundaries meaning in relationships, I thought loving someone meant being available 24/7," says Elena, a relationship coach. "Now I know that what is a boundary in a relationship actually strengthens the connection by preventing burnout and resentment."
Setting Boundaries at Work: Professional Protection
Work boundaries are increasingly important in our always-connected world. Setting personal boundaries at work might include:
Defining your work hours and availability
Clarifying role responsibilities
Establishing communication preferences
Creating physical workspace boundaries
Setting limits on workload
One client told me she created a humorous "Do Not Disturb" sign for her desk with different levels—from "Quick questions welcome" to "Unless the building is on fire, please email me instead!" Her lighthearted approach made boundary setting at work more comfortable for everyone.
Practical Methods for How to Establish Boundaries
Knowing you need boundaries and actually implementing them are two different challenges. Here are practical steps for how to create boundaries that stick:
1. Start with self-awareness: Identify your feelings of discomfort or resentment as boundary signals
2. Get clear on your needs: Define exactly what you require
3. Communicate directly: Express your boundaries clearly and calmly
4. Start small: Begin with less emotionally charged situations
5. Be consistent: Enforce your boundaries consistently
6. Expect resistance: Prepare for pushback and hold firm
7. Revise as needed: Adjust boundaries that aren't serving you well
Creating healthy boundaries doesn't happen overnight. Think of it as learning to play an instrument—awkward at first, but increasingly natural with practice.
How to Be Assertive When Saying No
For many, the biggest boundary challenge is learning how to kindly say no. Let's explore how to be more assertive with this essential skill.
Different Ways to Say No Politely
There are many other ways to say no that maintain both boundaries and relationships:
1. The gratitude approach: "Thank you for thinking of me, but I'm not able to take this on."
2. The honest explanation: "I'd love to help, but my schedule is already at capacity."
3. The alternative offer: "I can't do that, but here's what I can offer instead..."
4. The raincheck: "I can't right now, but I might be available after [specific date]."
5. The direct approach: "No, that doesn't work for me."
How to Deny Politely Without Guilt
Learning how to say no politely doesn't mean you need lengthy explanations or white lies. Most people respect a clear, kind refusal more than an insincere yes or a flaky commitment.
"I used to agonize over how can I say no without hurting feelings," shares Damon, a community volunteer. "Now I realize that saying no to things that drain me means I have more energy for the yeses that matter."
Sometimes, the most politely decline you can offer is simple and straightforward: "I'm sorry, but I won't be able to attend." Period!
Tools and Resources for Your Self-Advocacy Journey
Developing self-advocacy skills is an ongoing process. These resources can support your growth:
Personal Boundaries Worksheet and Handouts
A boundaries handout or personal boundaries worksheet can provide structure for your reflection. Look for worksheets on boundaries that prompt you to:
Identify areas where your boundaries are strong versus weak
Recognize boundary violations you've experienced
Practice boundary-setting language
Create strategies for maintaining boundaries under pressure
Many therapists and coaches offer worksheets on setting boundaries that you can use for self-guided work.
Boundary Setting Exercises
Try these practical exercises to strengthen your boundary-setting muscles:
1. The mirror practice: Rehearse assertive statements in front of a mirror
2. The boundary journal: Track boundary violations and your responses
3. The values clarification: Identify your core values to inform your boundaries
4. The role-play: Practice difficult conversations with a trusted friend
5. The daily check-in: Ask yourself, "What boundaries do I need to maintain today?"
Embracing Your Self-Advocacy Journey
Remember that advocating for self is a skill that develops over time. Like any meaningful change, it happens step by step, with both successes and setbacks along the way.
The self advocate meaning is ultimately about honoring your inherent worth. By embracing assertive personality traits and learning to set healthy boundaries, you create space for genuine connection, meaningful contribution, and personal well-being.
As you practice these skills, notice how your relationships transform. Those worth keeping will adapt and deepen, while connections built on unhealthy dynamics may fall away—making room for more fulfilling interactions.
What small step will you take today to advocate for yourself? Perhaps it's practicing one assertive statement, identifying a boundary that needs reinforcing, or simply reflecting on your needs. Whatever you choose, remember that each small act of self-advocacy builds momentum toward a more authentic and empowered life.
After all, if you don't advocate for yourself, who will?
Aphasia or Dysarthria? Learn the Difference Between These Communication Disorders
Aphasia affects over 3 million Americans and Canadians, causing difficulties with language comprehension and expression. This comprehensive guide explains the various types of aphasia, their causes, and how they impact daily communication
Aphasia is a complex language disorder that affects millions of people worldwide, impacting their ability to express themselves, understand others, and connect with the world around them. Whether caused by stroke, injury, or progressive neurological conditions, aphasia fundamentally changes how someone communicates—often suddenly and without warning. This comprehensive guide explores the various kinds of aphasia, how they differ from other speech disorders, and what happens in the brain when language abilities are disrupted.
What Is Aphasia? Definition and Meaning
Aphasia is a language disorder that impairs a person's ability to process and use language. Unlike other speech disorders, aphasia specifically affects language skills rather than just the physical ability to produce speech sounds. People with aphasia may struggle to speak, understand speech, read, or write, depending on which areas of the brain are affected.
The term "aphasia" comes from Greek, meaning "speechlessness" or "without speech," though most people with aphasia retain some language abilities. It's important to understand that aphasia doesn't affect intelligence—people with aphasia know what they want to say but struggle to access or organize the words needed to express themselves.
Consider Sarah, a retired teacher who suffered a stroke at age 65. Before her stroke, Sarah was articulate and loved crossword puzzles. Afterward, she could understand most conversations but struggled to find common words. "I know what I want to... want to..." she would say, gesturing in frustration as the word remained just out of reach. This word-finding difficulty is one of the most common and frustrating symptoms of aphasia.
Types of Aphasia: Understanding Different Communication Challenges
Aphasia manifests in various ways, and neurologists categorize it into several types based on the symptoms and affected brain regions. The main classifications include expressive aphasia, receptive aphasia, anomic aphasia, and global aphasia.
Expressive Aphasia (Broca's Aphasia)
Expressive aphasia, also called Broca's aphasia or motor aphasia, affects a person's ability to produce language. People with this condition understand what others say fairly well but struggle to form complete sentences themselves. Their speech is typically non-fluent, characterized by short, simplified phrases that require great effort.
James, a 58-year-old accountant, developed expressive aphasia after a stroke. His typical sentence might be: "Want coffee... cup... please." He understands questions and can nod or shake his head appropriately but becomes frustrated when trying to explain complex thoughts. Expressive aphasia results from damage to the Broca area, located in the frontal lobe of the left hemisphere of the brain. This region is crucial for speech production and processing grammar.
Receptive Aphasia (Wernicke's Aphasia)
Receptive aphasia, also known as Wernicke's aphasia or sensory aphasia, presents almost as the opposite of expressive aphasia. People with this type produce fluent speech but have difficulty understanding what others say to them. Their own speech may sound normal in rhythm and grammar but often contains irrelevant or made-up words, making it difficult for others to follow.
Maria, a 72-year-old grandmother, experienced receptive aphasia following a stroke. She speaks fluently, with normal intonation, but her sentences often don't make sense: "I went to the market and the flowers were singing to the blue sky of trees." When family members speak to her, she frequently misunderstands or responds inappropriately. Receptive aphasia stems from damage to Wernicke's area in the temporal lobe of the left brain hemisphere, the region responsible for language comprehension.
Anomic Aphasia (Nominal Aphasia)
Anomic aphasia, sometimes called nominal aphasia, is characterized by persistent difficulty finding words, particularly nouns and verbs. People with anomic aphasia typically understand speech well and can produce grammatically correct sentences but struggle to find the specific words they want to use.
This is often described as having words "on the tip of your tongue" all the time. Someone with anomic aphasia might say, "Can you hand me that... that thing you use to... you know, when you eat soup," when trying to ask for a spoon. This type of aphasia can be especially frustrating because the person knows exactly what they want to say but cannot access the word.
Global Aphasia
Global aphasia is the most severe form, affecting all aspects of language processing. People with global aphasia have significant impairments in both expressing and understanding language. They typically can produce only a few recognizable words and understand little or no spoken language.
Robert, a formerly eloquent attorney, experienced global aphasia following a massive stroke. He can only say a few words like "yes," "no," and "help," regardless of what he wants to express. He also struggles to understand what others say to him, making communication extremely challenging. Global aphasia results from extensive damage to multiple language areas of the brain.
Primary Progressive Aphasia (PPA)
Unlike other types of aphasia that occur suddenly after brain injury or stroke, primary progressive aphasia (PPA) develops gradually over time. It's a neurodegenerative condition in which language capabilities slowly deteriorate.
In the early stages, symptoms might be subtle—occasional word-finding problems or mild comprehension difficulties. As the disease progresses, communication becomes increasingly difficult. There are several subtypes of PPA, each affecting different aspects of language. This condition differs from typical aphasia because it's degenerative rather than caused by a single event like a stroke.
Aphasia vs. Other Speech Disorders: Understanding the Differences
People often confuse aphasia with other conditions that affect speech, particularly dysarthria and dysphasia. Understanding the differences helps in proper diagnosis and treatment.
Aphasia vs. Dysarthria
While aphasia is a language disorder affecting language processing, dysarthria is a motor speech disorder. Dysarthria occurs when the muscles used for speech are weak or difficult to control. People with dysarthria know what they want to say and can process language normally, but they have trouble physically forming words correctly.
The defining characteristic of dysarthria is slurred speech, where words sound mumbled or unclear. Other symptoms might include speaking too slowly or quickly, changing voice pitch, or speaking too softly. Different types of dysarthria exist, including ataxic dysarthria and hypokinetic dysarthria, each with distinct speech patterns based on which neurological systems are affected.
Compare John and Michael's experiences: John has aphasia and can physically form sounds correctly but struggles to find words or understand language. Michael has dysarthria—he knows exactly what he wants to say and understands others perfectly, but his speech sounds slurred because he can't control his speech muscles properly.
Aphasia vs. Dysphasia
The terms "aphasia" and "dysphasia" are often used interchangeably, especially in different parts of the world. "Dysphasia" literally means "impaired speech" while "aphasia" means "no speech," though in practice, both terms refer to language impairments resulting from brain damage. In the United States, "aphasia" is more commonly used, while "dysphasia" is more prevalent in European countries.
Aphasia vs. Aphagia
Despite sounding similar, aphagia (dysphagia) is entirely different from aphasia. Aphagia refers to the inability to swallow, a physical condition affecting the throat muscles, while aphasia affects language processing in the brain. This distinction highlights the importance of precise terminology in medical discussions.
The Neuroscience of Language: Brain Regions and Aphasia
Understanding aphasia requires knowledge of how the brain processes language and which regions are involved.
Broca's Area: The Production Center
Broca's area, located in the left frontal lobe, is crucial for speech production. Named after French physician Paul Broca, who identified its function in the 1860s, this region helps coordinate the complex muscle movements needed for speaking and processes grammar. Damage to Broca's area results in expressive aphasia, where speech production is labored and simplified.
Wernicke's Area: The Comprehension Hub
Wernicke's area, situated in the left temporal lobe, primarily deals with language comprehension. Named after Carl Wernicke, a German neurologist, this region helps us understand the meaning of spoken and written language. When Wernicke's area is damaged, a person develops receptive aphasia, characterized by fluent but often meaningless speech and difficulties understanding others.
Language Network: Beyond Broca and Wernicke
Modern neuroscience has revealed that language processing involves a complex network of brain regions beyond just Broca's and Wernicke's areas. The arcuate fasciculus, a bundle of nerve fibers, connects these two regions and is essential for repeating words and phrases. Additional areas in the temporal, parietal, and frontal lobes contribute to various aspects of language processing, from recognizing words to understanding context.
This explains why aphasia can manifest in so many different ways—damage to different parts of this intricate network results in different patterns of language impairment.
Causes of Aphasia: When Communication Systems Break Down
Aphasia always results from damage to the language centers of the brain, but this damage can occur in several ways.
Stroke and Aphasia
Stroke is the most common cause of aphasia, accounting for about 25-40% of stroke survivors experiencing some form of aphasia. During a stroke, blood flow to part of the brain is interrupted, either by a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). When brain cells in language areas don't receive oxygen, they begin to die, resulting in language impairments.
The acronym "CVA with aphasia" is often seen in medical records, referring to a cerebrovascular accident (stroke) that has resulted in aphasia. The severity and type of aphasia depend on the location and extent of brain damage.
Traumatic Brain Injury
Traumatic brain injuries from accidents, falls, or other physical trauma can damage language centers and cause aphasia. The nature of the language difficulties depends on which brain regions are affected.
Brain Tumors
Tumors growing in or pressing on language areas of the brain can cause aphasia. Sometimes, aphasia symptoms are the first indication of a brain tumor, prompting diagnostic tests.
Infections
Certain infections that affect the brain, like encephalitis, can cause inflammation and damage to language centers, resulting in aphasia.
Degenerative Conditions
Primary progressive aphasia (PPA) is related to neurodegenerative diseases like frontotemporal dementia or Alzheimer's disease. In these cases, the aphasia develops gradually as the condition progresses.
Common Symptoms and Daily Challenges
Aphasia manifests through various symptoms that can significantly impact daily life.
Word-Finding Difficulties
One of the most common and frustrating symptoms across different types of aphasia is difficulty finding words. People with aphasia often know what they want to say but can't access the specific words needed. This symptom is particularly predominant in anomic aphasia but occurs in most types to some degree.
David, a 62-year-old engineer with mild aphasia, describes it this way: "It's like having a filing cabinet where someone has rearranged all the folders. The information is there, but I can't find it when I need it."
Mixing Up Words When Talking
Many people with aphasia experience paraphasias—substituting one word for another or creating nonsensical words. Someone might say "chair" when they mean "table" or create a nonexistent word like "blimpet" when trying to say "blanket". This symptom can be confusing and frustrating for both the person with aphasia and their conversation partners.
Speech Fluency Changes
Depending on the type of aphasia, a person's speech fluency may change dramatically. Those with expressive aphasia typically have non-fluent speech—halting, effortful, and consisting of short phrases. Conversely, those with receptive aphasia often maintain fluent speech that sounds normal in rhythm but may lack meaningful content.
Comprehension Difficulties
Difficulty understanding spoken language is a key symptom, especially in receptive and global aphasia. This can range from missing subtle details to being unable to follow basic instructions or conversations. Some people with aphasia report that speech sometimes sounds like a foreign language or "gibberish" to them.
Reading and Writing Challenges
Aphasia typically affects all language modalities, including reading and writing. A person who previously enjoyed reading novels might suddenly find text incomprehensible, or someone who wrote regularly might struggle to compose even simple messages. These challenges often reflect the same patterns as their spoken language difficulties.
Sudden Onset in Elderly
Sudden slurred speech or language difficulties in elderly people should be taken seriously as a potential sign of stroke requiring immediate medical attention. While aphasia can affect people of any age, its most common cause—stroke—occurs more frequently in older adults.
Living With Aphasia: Strategies and Support
Despite the significant challenges aphasia presents, many people find ways to improve their communication and quality of life.
Speech-Language Therapy
Speech-language therapy is the primary treatment for aphasia. Therapists work with individuals to improve language skills, develop alternative communication strategies, and maximize remaining abilities. The effectiveness of therapy varies depending on the cause, type, and severity of aphasia, as well as how quickly treatment begins.
Therapy approaches include:
Constraint-induced language therapy, which "forces" the use of spoken language
Melodic intonation therapy, which uses musical elements to improve speech
Group therapy, which provides practice in social settings
Computer-assisted therapy programs
Communication Strategies
People with aphasia and their families often develop personalized strategies to improve communication, such as:
Using gestures, writing, or drawing to supplement speech
Creating communication books with important words or pictures
Using specialized apps designed for people with aphasia
Allowing extra time for communication without rushing
Focusing on one topic at a time with clear transitions
Support Networks
Support groups specifically for people with aphasia and their families provide valuable emotional support and practical advice. Connecting with others who understand the challenges of aphasia can reduce isolation and share coping strategies. National organizations like the National Aphasia Association offer resources, information, and community connections.
Conclusion
Aphasia represents much more than a medical diagnosis—it's a profound life change that affects how people connect with others and express their thoughts, needs, and personalities. Understanding the different kinds of aphasia and how they affect communication is crucial for healthcare providers, family members, and society at large.
While aphasia presents significant challenges, advances in rehabilitation techniques, assistive technologies, and growing awareness are helping many people with aphasia find new ways to communicate effectively. With appropriate support and understanding, people with aphasia can continue to participate meaningfully in relationships, activities, and communities.
The journey with aphasia is different for everyone, shaped by the type and severity of the condition, the cause, available treatments, and personal factors. What remains constant is the fundamental human need to connect through communication—a need that continues even when the pathways to expression change.
The Complete Guide to Raspy Voices: How to Enhance or Reduce your Huskiness
Ever wondered why some voices sound deliciously husky while others develop unwanted raspiness? This comprehensive guide explores everything from the science behind raspy voices to practical solutions for either developing or healing that distinctive vocal quality. Whether you're a performer seeking that special edge or someone looking to restore vocal clarity, you'll find actionable advice backed by vocal health expertise.
Have you ever woken up sounding like you've been gargling gravel all night? Or perhaps you've admired the sultry, textured tones of singers like Stevie Nicks or Tom Waits? Raspy voices - they're fascinating, sometimes desirable, occasionally concerning, but always distinctive. As someone who's personally battled with vocal raspiness after late-night karaoke sessions (my rendition of "Sweet Child O' Mine" has consequences!), I've learned there's much more to this vocal quality than meets the ear.
What Exactly Is a Raspy Voice?
A raspy voice sounds rough, hoarse, or gravelly - like sandpaper against wood compared to the smooth glide of silk. This distinctive quality happens when your vocal cords don't close completely during speech or singing, allowing extra air to escape and creating that characteristic husky sound. Think of it as a partially closed door that rattles and vibrates when air passes through, rather than opening and closing cleanly.
Many people wonder, "Do I have a raspy voice?" If you've been told your voice has a scratchy, husky, or gravelly quality, then yes - you might naturally possess what others try to artificially create. Just like fingerprints, each person's raspy voice has its own unique character and charm.
The Attraction Factor of Raspy Voices
Are raspy voices attractive? For many people, absolutely! There's something undeniably captivating about a voice with texture and character. Research suggests that voices with some raspiness are often perceived as more experienced, authoritative, and even sensual. Like a well-worn leather jacket compared to a brand new one, a voice with some "edge" often carries more personality and story.
Many famous personalities, from actors like Scarlett Johansson to musicians like Bob Dylan, have turned their distinctive raspy voices into career assets. Their voices don't just communicate words – they convey emotion, history, and uniqueness in ways perfectly smooth voices sometimes cannot.
Why Is My Voice Raspy? Common Causes Explained
Natural and Genetic Factors
Some people are simply born with vocal anatomy that produces a naturally raspy sound. Just as some people have naturally curly hair while others have straight, vocal characteristics can be an inherited trait. Your vocal folds' thickness, your larynx size, and even the shape of your throat can all contribute to your voice's natural timbre.
Temporary Causes of Raspiness
If you're wondering, "Why is my voice raspy all of a sudden?" several temporary factors might be at play:
Dehydration acts like drought on farmland – your vocal cords need moisture to function optimally, and without it, they become dry and irritated. Imagine trying to slide smoothly on a dry waterslide versus one that's properly lubricated with water. That's the difference hydration makes to your vocal cords.
Excessive talking or yelling is like running a marathon without training – it exhausts your vocal cords. After cheering at a football game or teaching back-to-back classes, your voice might protest with raspiness.
Many people ask, "Why is my voice raspy after drinking?" Alcohol dehydrates your entire body, including those sensitive vocal cords. Combined with the tendency to talk louder in social settings, that post-party hoarseness makes perfect sense.
For parents wondering, "Can teething cause a raspy voice in my child?" – the answer is indirectly yes. Teething can cause excess mucus, discomfort, and crying, all potentially leading to vocal strain.
Medical Conditions That Cause Raspy Voices
Several health conditions can lead to vocal raspiness:
Allergies affect millions of Americans, and many ask, "Can allergies cause a raspy voice?" Yes – postnasal drip irritates the vocal cords, while throat clearing damages them further. Do allergies cause raspy voice consistently? They certainly can, especially during high pollen seasons.
Acid reflux is like a stealth attacker, often striking while you sleep. Stomach acid creeps up and irritates your vocal cords, leaving you wondering why your morning voice sounds like you've been smoking for decades.
Speaking of which – does smoking give you a raspy voice? Unequivocally yes. Smoking damages vocal cords through heat, chemicals, and irritation. Does smoking make your voice raspy permanently? With long-term use, the changes can indeed become permanent.
And for the curious: does smoking marajuana make your voice raspy? It can, through similar mechanisms of heat and irritation, though typically to a lesser degree than tobacco.
How to Get a Raspy Voice (If You Want One)
Many people, particularly performers, wonder how to make their voice raspy. If you're among those asking, "How can I get a raspy voice?" or "How to get a raspy voice permanently," here are some approaches (though I must emphasize health comes first):
Safe Methods to Develop Raspiness
Vocal techniques can help you learn how to make your voice sound raspy without damage. Voice coaches often teach controlled techniques that simulate raspiness while protecting vocal health. This is like learning to create the illusion of painting texture without actually scratching the canvas.
Hydration plays a role here, too—slight dehydration can create temporary raspiness, though I don't recommend this as a regular practice.
For those wondering how to get a raspy singing voice specifically, working with a voice therapist or vocal coach is your safest bet. They can teach techniques like vocal fry and controlled breathiness that create texture without strain.
What NOT To Do
While many search for "how to make your voice raspy fast," I strongly caution against harmful methods. Screaming, whispering aggressively, or deliberately irritating your throat can cause lasting damage. It's like trying to get a tan by getting a sunburn – the short-term result isn't worth the long-term damage.
Does coffee make your voice raspy? Temporarily it might, due to mild dehydration, but it's not a healthy long-term strategy.
How to Fix a Raspy Voice (If You Don't Want One)
For those asking, "How to get rid of a raspy voice," or "How to cure a raspy voice fast," here are effective approaches:
Immediate Relief Strategies
Hydration is your voice's best friend. Drinking plenty of water throughout the day keeps your vocal cords lubricated and healthy. Like a garden needs consistent watering rather than occasional flooding, regular hydration works better than chugging water only when symptoms appear.
Steam inhalation can provide quick relief for irritated vocal cords. The warm, moist air is like a gentle massage for your voice. Imagine the soothing feeling of a warm compress on sore muscles – that's what steam does for strained vocal cords.
Voice rest might not be what you want to hear, but it's often what you need to hear. Giving your voice a break is like taking a day off after intense exercise – it allows for recovery and prevents further damage.
Long-term Solutions and Lifestyle Changes
If you're searching for "how to fix raspy voice" for the long term, consider these adjustments:
Avoiding irritants like smoke, excessive alcohol, and screaming seems obvious, but it's worth emphasizing. These are to your voice what sandpaper would be to your skin – unnecessary friction that causes damage.
Proper speaking techniques can transform vocal health. Learning to speak from your diaphragm rather than your throat reduces strain, like learning to lift with your legs instead of your back.
For chronic issues, especially if you're wondering "why is my voice raspy for weeks," medical intervention might be necessary. ENT specialists can identify and treat underlying conditions that home remedies can't address.
Special Situations and FAQs
Morning Raspiness
Many people wonder, "How to get rid of raspy voice in the morning?" Morning voice roughness is often caused by overnight dehydration or reflux. Keeping water by your bed, elevating your head slightly while sleeping, and avoiding late-night eating can help dramatically.
Raspy Voice When Sick
For those asking "how to fix raspy voice when sick," gentle care is key. Extra hydration, warm (not hot) teas with honey, and complete voice rest can speed recovery.
Raspy Voice While Singing
Performers often search for "how to get rid of raspy voice when singing" or conversely, "how to get a raspy singing voice." The answer depends on your goal, but vocal warm-ups, proper technique, and consistent training are universal foundations. Like athletes who practice specific movements until they become second nature, singers can train their voices to either eliminate or control raspiness.
When to See a Doctor
How long does a raspy voice last typically? If it's due to a cold or vocal strain, usually no more than 1-2 weeks. Anything longer warrants medical attention. A persistent raspy voice, especially when accompanied by pain, difficulty swallowing, or a feeling of a lump in the throat, should never be ignored. These symptoms are like check engine lights on your car's dashboard – they're warnings that merit professional evaluation.
The Cultural Impact of Raspy Voices
From Lauren Bacall's iconic "You know how to whistle, don't you?" to the distinctive tones of public figures like RFK Jr. (many search "why does RFK have a raspy voice" – in his case, it's reportedly due to a condition called spasmodic dysphonia), raspy voices have left their mark on our cultural landscape.
When people ask, "Do guys like raspy voices?" or search for information about voice attractiveness, they're tapping into something primal about human communication. Voices carry not just words but personality, emotion, and uniqueness – and raspiness adds a layer of complexity that many find appealing.
Embracing Your Voice, Whatever Its Texture
Whether you're looking to develop a raspy voice or hoping to smooth one out, remember that your voice is as unique as your fingerprint. Like handwriting, it carries your personality and can evolve with time and attention.
For some, a raspy voice is a cherished characteristic that sets them apart. For others, it's an unwanted symptom they'd like to address. Whichever camp you fall into, understanding the mechanisms behind vocal raspiness empowers you to make informed choices about your vocal health and expression.
Remember, voice is more than just sound – it's your personal instrument for connecting with the world. Treat it with care, whatever its natural texture may be.
Mastering Communication in Ontario: A Guide to Speech, Voice, and Language
From navigating small talk to overcoming stutters, effective communication shapes our daily lives. This guide dives into speech therapy, voice training, and accent improvement in Toronto, offering actionable tips and local resources like Two Can Talk and The Voice Clinic.
Have you ever felt your words stumble during small talk, or noticed your voice waver in a meeting? Whether it’s a stutter, a stammer, or mumbling, communication challenges can feel isolating. But in Toronto, a city buzzing with diverse voices, help is closer than you think. From speech therapy clinics to accent reduction classes, let’s explore how to transform your communication skills—one word at a time.
What Are Stutters and Stammers?
Definitions and Differences
Stutter Meaning: A speech disorder involving repetitions, prolongations, or blocks in sounds (e.g., “c-c-can you hear me?”).
Stammer Definition: Often used interchangeably with stuttering, though some define it as irregular pauses or hesitations.
Stuttering vs. Stammering: While similar, stuttering is more commonly used in North America, whereas stammering is preferred in the UK.
Example: Jordan, a Toronto-based sales professional, avoided workplace communication due to his stammer. After enrolling in speech therapy at Two Can Talk, he learned breathing techniques to manage his speech flow.
Speech Therapy in Toronto: Your Questions Answered
Q&A: Common Queries
Q: What does a speech therapist do?
A: Speech-language pathologists (SLPs) assess and treat disorders like stutters, lisps, and dysphonia. At clinics like The Speech Clinic Toronto, they tailor exercises to improve clarity and confidence.
Q: How is talk therapy different from psychotherapy?
A: Talk therapy (psychotherapy) focuses on mental health, while speech therapy targets communication mechanics. However, anxiety from stuttering might involve both!
Q: Can adults benefit from voice lessons?
A: Absolutely! Tiffany Wong, a Toronto vocal coach, helps clients refine their singing *and* talking voices through adult vocal lessons.
Accent Reduction and Voice Training
Accent Improvement in Toronto
Whether it’s an international or regional accent, many seek accent reduction classes for personal or professional reasons.
Comparison:
Accent Elimination vs. Accent Reduction: Elimination aims to erase an accent, while reduction focuses on clarity. Most Toronto programs, like Accent on Toronto, prioritize mutual intelligibility over conformity.
Anecdote: Maria, an immigrant from Spain, enrolled in accent reduction training at Language Therapy Toronto to boost her workplace communication. Her team now describes her as “clear and commanding.”
Voice Rehabilitation for Dysphonia
Conditions like functional dysphonia or muscle tone dysphonia (MTD) strain vocal cords. Clinics like The Voice Clinic Toronto offer vocal rehabilitation, combining speech therapy and exercises to restore vocal health.
Small Talk: The Art of Connection
What Is Small Talk?
Small talk is light, informal conversation to build rapport—think chatting about the weather or weekend plans. But for those who stutter or mumble, it can feel daunting.
How to Make Small Talk:
1. Ask Open-Ended Questions: “What brought you to Toronto?”
2. Listen Actively: Nodding and paraphrasing shows engagement.
3. Practice with a Pro: Speech therapists at Toronto Adult Speech Clinic role-play scenarios to build confidence.
Anecdote: After language therapy for adults at SLP Therapy Toronto, Emma went from dreading networking events to hosting them!
Singing vs. Talking: Surprising Overlaps
Voice Lessons for Speech and Song
Toronto’s singing coaches, like those at Vocal Lessons Toronto, often work with clients on both artistic and everyday communication.
Comparison:
Singing Voice vs. Speaking Voice: Singing requires controlled breath and pitch, while talking relies on natural rhythm. However, techniques from voice training (e.g., diaphragmatic breathing) benefit both.
Case Study: A client with a lisp saw improvement after combining speech therapy Etobicoke sessions with singing lessons to strengthen articulation.
Workplace Communication: From Mumbling to Leadership
Why Communication Matters at Work
Mumbled presentations or anxiety during meetings can hinder careers. Programs like public speaking lessons Toronto tackle these challenges.
Tips:
Record yourself or ask a friend “Can you hear me?” to identify mumbling.
Enroll in workplace communication workshops to practice assertiveness.
Local Toronto Resources Spotlight
Speech and Language Clinics
Two Can Talk - Speech Therapy: Specializes in stuttering and language therapy for adults.
The Voice Clinic Toronto: Offers vocal rehabilitation for dysphonia and MTD.
Speech Therapy Etobicoke: Affordable rates for accent reduction and lisps.
Voice and Singing Coaches
Tiffany Music Therapy: Blends singing and speech exercises for holistic growth.
Adult Vocal Lessons Toronto: Perfect for refining pitch and projection.
When to Seek Help: Red Flags
Chronic throat strain (muscle tone dysphonia).
Avoidance of social interactions due to stuttering.
Colleagues frequently ask, “Can you repeat that?”
Final Thoughts: Finding Your Voice in Toronto and Guelph
From the bustling streets of Thornhill to downtown Toronto, communication shapes our connections. Whether you’re exploring accent massage therapy (just kidding) or recovering from functional dysphonia, remember: every voice deserves to be heard.
Take Action Today:
Book a consultation at Speech Language Clinic Toronto.
Join a small talk workshop to polish conversational skills.
Your words matter—let Ontario’s experts help you share them confidently.