Stuttering, Stammering and Cluttering
Is it a stutter or a stammer? Explore the nuances of speech disfluencies, practical solutions, and inspiring stories to help you navigate fluency challenges.
Stutter vs Stammer: Breaking Down Disfluencies and Finding Solutions
Picture this: You’re introducing yourself at a meeting, and your words suddenly freeze—like a glitch in your speech. For millions worldwide, this experience is part of daily life. Whether called a stutter, stammer, or disfluency, interruptions in speech flow are more common than you might think. Let’s unravel these terms, share relatable stories, and explore actionable strategies for clearer communication.
Stutter vs Stammer: What’s the Difference?
The terms “stutter” and “stammer” often spark confusion. Here’s the simple truth: they’re regional variations of the same concept. In the U.S., “stuttering” is preferred, while the U.K. often uses “stammering.” Both describe disfluent speech—repetitions, prolongations, or blocks in sounds (e.g., “I n-n-need that report” or “Sssssaturday”).
But nuances exist:
Stuttering: Typically refers to sound/syllable repetitions (*“b-b-bike”*) or tense pauses.
Stammering: Sometimes associated with broader hesitations or word-finding struggles.
Example: Meet Alex, a podcast host who stutters. He practices pacing his speech and uses gentle breathing techniques to navigate tricky words. Meanwhile, Priya, a teacher in London, describes her stammer as “words tripping over each other” when she’s stressed.
Types of Disfluencies: Beyond Stuttering
Not all disfluencies are alike. Here’s a quick guide:
Repetitions: “Let’s go to the- the- the park.”
Prolongations: “Sssssssee you later!”
Blocks: Silent struggle before a word (e.g., “… [pause] tomorrow”).
Interjections: “Um, I think, uh, we should leave.”
Cluttering, a lesser-known fluency disorder, involves rapid, irregular speech that sounds “jumbled.” Think of it as speech that’s too fast for the mouth to keep up. For instance: “Heycanwegotothemeetnow?” (Translation: “Hey, can we go to the meeting now?”).
What Causes Stuttering and Stammering?
Childhood Stuttering
About 5% of children stutter during speech development, often starting between ages 2–6. While most outgrow it, 1% carry it into adulthood. Causes may include:
Genetics: 60% of people who stutter have a family member who does too.
Brain Differences: Slight variations in speech-motor control areas.
Anecdote: Eight-year-old Liam’s parents noticed his stutter during a growth spurt. With early intervention, he now uses “easy onsets” (gentle voice starts) to smooth his speech.
Adult Stammering
Adult-onset stammering is rarer and often linked to:
Neurological Events: Strokes or traumatic brain injuries.
Psychological Stress: Anxiety exacerbating latent disfluencies.
Example: After a car accident, Maria developed a stammer. Speech therapy helped her regain confidence through mindfulness and rhythmic speaking exercises.
How to Manage Disfluencies: Practical Strategies
While there’s no universal “cure” for stuttering or stammering, these approaches can reduce disfluencies:
1. Speech Therapy Techniques
Slow Speech: Stretching vowels (“Haaappy birthday”) to ease tension.
Breathing Exercises: Coordinating breath with phrases.
Electronic Devices: Delayed auditory feedback (DAF) tools that “echo” speech, slowing pace.
2. Mindset Shifts
Avoid Avoidance: Skipping words or social events worsens anxiety.
Self-Compassion: As podcaster Alex says, “My stutter is part of my voice—not a flaw.”
3. Addressing Cluttering
Pacing: Using a metronome app to regulate speech rate.
Over-articulation: Exaggerating sounds for clarity.
Anecdote: Comedian Drew Lynch, who stutters, turned his disfluency into a punchline: “I’m not nervous—my brain just buffering!”
Can Stuttering Be “Fixed”?
While some achieve near-fluency, the goal is often effective communication, not perfection. Techniques like speech therapy, support groups (e.g., the National Stuttering Association), and technology (e.g., SpeechEasy devices) empower individuals to thrive.
Key Takeaway: Progress, not perfection, is the aim.
FAQ
Q: How do I stop stammering in high-pressure situations?
A: Practice grounding techniques: pause, breathe, and restart the phrase.
Q: Is cluttering linked to ADHD?
A: Sometimes—cluttering often co-occurs with attention disorders.
Q: Can anxiety cause stuttering? It doesn’t *cause* it, but stress can amplify disfluencies.
Q: How to help a child who stutters?
A: Listen patiently, avoid finishing their sentences, and consult a speech-language pathologist.
Whether you stutter, stammer, or clutter, your voice matters. With patience and support, fluency challenges can become stepping stones, not roadblocks. 🗣️💛
What Are Speech Sound Disorders?
Ever wondered how common speech errors are? From rhotacism to phonological disorders, discover the facts, examples, and solutions for clearer communication.
How Common Are Speech Errors? Insights into Rhotacism, Articulation, and Beyond
Have you ever tripped over a word, swapped a sound, or felt self-conscious about a lingering speech quirk? You’re not alone. Speech errors are far more common than most people realize—and they don’t just affect children. Let’s dive into the fascinating world of speech sound challenges, from the well-known rhotacism to the nuances of articulation vs. phonological disorders.
Speech Errors in Adults: More Common Than You Think
While many associate speech errors with childhood development, adults aren’t immune. Studies suggest that 5% of adults live with residual speech sound disorders, such as difficulty pronouncing specific sounds like R (rhotacism) or L. Take Sarah, a marketing executive who avoids saying “rural” in meetings because her r sounds come out as w (“wuh-ral”). Her experience reflects a classic rhotacistic speech impediment, a type of articulation disorder.
Rhotacism: When R Becomes a Challenge
Rhotacism—often humorously dubbed “the Elmer Fudd effect” (think “wabbit” instead of “rabbit”)—is one of the most recognizable speech errors. It occurs when the R sound is distorted, substituted (e.g., R → W), or omitted entirely. While common in children, some adults retain this pattern. Celebrities like Jonathan Ross have openly discussed their rhotacism, proving it doesn’t have to hold you back.
But rhotacism is just one piece of the puzzle. Speech errors can stem from:
Articulation disorders: Mechanical difficulties producing sounds (e.g., lisping th for s).
Phonological disorders: Cognitive challenges organizing speech sounds into patterns (e.g., dropping all ending consonants: “ca” for “cat”).
Articulation vs. Phonology: What’s the Difference?
Imagine articulation as the how of speech (physical sound production) and phonology as the rules (sound patterns in language).
Articulation Disorder vs. Phonological Disorder
Articulation
Struggles with specific sounds (e.g., R or L).
Example: “Wed” for “red” (rhotacism).
Phonology
Struggles with sound patterns (e.g., fronting: “tup” for “cup”).
Example: “Wed” for “red” (rhotacism). | Example: “Tat” for “cat” (replacing back sounds with front ones).
A child who says “wabbit” has an articulation issue. A child who says “gog” for “dog” (swapping d and g) may have a phonological processing disorder.
The Articulation Hierarchy: Building Blocks of Clear Speech
Speech-language pathologists use the articulation hierarchy to guide therapy:
1. Isolation: Mastering the sound alone (e.g., “rrrr”).
2. Syllables: Combining with vowels (“ra, re, ri”).
3. Words: “Rabbit,” “carrot.”
4. Sentences: “The rabbit runs rapidly.”
5. Conversation: Generalizing the sound in daily speech.
For adults, this process might focus on refining lingering habits. James, a teacher with a mild lisp, practiced s sounds using tongue twisters (“Sally sells seashells”) during articulation therapy—and now speaks confidently in class.
When L or R Won’t Cooperate
Ever met someone who says “yeg” instead of “leg”? Difficulty pronouncing L (a condition where people can’t say the letter L) often stems from tongue placement issues. Similarly, substituting R with W (common in rhotacism) can persist into adulthood without intervention.
Finding Solutions: Therapy and Beyond
Whether it’s articulation therapy for specific sounds or strategies for phonological disorders, help is available. Techniques might include:
Visual aids (mirrors for tongue placement).
Auditory discrimination exercises (“Is this ‘wing’ or ‘ring’?”).
Play-based drills for children.
The Takeaway: Progress Over Perfection
Speech errors are human—and treatable. If you or someone you know struggles with sounds like R, L, or broader patterns, a speech-language pathologist can tailor a plan using the articulation hierarchy or phonological approaches.
FAQ
Q: How common is rhotacism in adults?
A: While exact numbers vary, studies suggest 2-3% of adults have residual R errors.
Q: What’s the difference between articulation and phonological disorders?
A: Articulation is about physical sound production; phonology involves language rules.
Q: Can adults improve speech errors?
A: Absolutely! Targeted therapy can yield significant progress.
Embrace the journey to clearer communication—it’s never too late to find your voice. 💬
Find a Language Therapist in Guelph or Toronto
Struggling with communication? Learn how speech therapy in Toronto and Guelph can help adults and children unlock their potential with personalized, evidence-based care.
Unlock Your Voice: The Power of Speech Therapy in Toronto & Guelph
Communication is the heartbeat of human connection. Whether it’s sharing a story, expressing emotions, or navigating daily tasks, our communication ability shapes our lives. But for many adults and children in Toronto, challenges like stuttering, aphasia, or language delays can feel like barriers. That’s where speech therapy in Toronto steps in—a lifeline for those seeking to reclaim their voice.
Why Speech Therapy Matters: A Toronto Success Story
Take Sarah, a 32-year-old marketing professional in Toronto. After a stroke left her with aphasia, she struggled to find words mid-conversation. Frustrated but determined, she turned to a language therapist in Toronto specializing in adult rehab. Through tailored SLP therapy sessions—combining exercises, technology, and compassion—Sarah regained confidence in her speech. “It wasn’t just about words,” she says. “It was about rebuilding *me*.”
Stories like Sarah’s highlight the transformative role of speech language pathology in Ontario. Whether it’s post-stroke recovery, accent modification, or childhood articulation issues, certified speech pathologists in Toronto use evidence-based strategies to meet individual needs.
Online Speech Therapy: Flexibility Meets Expertise
Gone are the days of commuting through Toronto traffic for appointments. Online speech therapy offers the same quality care from the comfort of home. Imagine a busy parent helping their child practice language skills via interactive games on a screen, guided by a speech therapist in Toronto in real-time. Or an adult refining their presentation skills through virtual sessions tailored to their schedule.
Studies show online language therapy is just as effective as in-person sessions for many conditions. Plus, it breaks down geographic barriers—ideal for clients in remote parts of Ontario or those balancing hectic routines.
Speech Therapy for Adults: It’s Never Too Late
Many assume speech therapy is only for kids, but adults make up a growing portion of clients at Toronto speech therapy clinics. Consider these scenarios:
A professional seeking language therapy for adults to improve clarity in workplace presentations.
A senior recovering from Parkinson’s disease working on vocal strength.
An immigrant refining English pronunciation to feel more confident socially.
Speech pathologists in Toronto and Guelph use tools like voice analysis software, cognitive-linguistic exercises, and even singing techniques to help adults thrive.
Choosing the Right Toronto Speech Therapy Clinic
With so many options, how do you pick the best fit? Look for:
1. Certified SLPs in Toronto & Guelph: Ensure therapists are licensed with Speech-Language Pathology Ontario (CASLPO)
2. Personalized Plans: Avoid one-size-fits-all approaches. Your goals should drive the therapy.
3. Flexible Formats: Clinics offering both online speech language therapy and in-person sessions provide convenience.
Pro tip: Many clinics offer free consultations. Use this to ask questions like, “Have you worked with cases similar to mine?” or “What’s your success rate?”
Final Thoughts: Your Voice Deserves to Be Heard
Whether you’re exploring SLP therapy for yourself or a loved one, remember that progress is possible at any age. Toronto’s vibrant network of speech therapists and clinics—both online and in-person—is ready to help you communicate with clarity and confidence.
Ready to take the first step? Reach out to a speech pathologist in Toronto or Guelph today and start your journey toward stronger communication.
How To Get Rid Of A Lisp
A lisp can feel like a stubborn typo in your speech—but it doesn’t have to be permanent. Explore the science behind lisps, actionable tips for improvement, and inspiring success stories.
What is a Lisp? Your Guide to Causes, Corrections, and Confidence
Picture this: A 7-year-old proudly declares they want to be a “thpace athtronaut” when they grow up. Their parents chuckle at the adorable mispronunciation, but over time, that endearing “th” sound lingers. For some, this quirk becomes a lifelong companion; for others, it fades with practice. Lisps—those slippery “s” and “z” sounds that twist words like “sun” into “thun”—are one of the most common speech quirks. But what exactly is a lisp? Why do they happen, and can they be corrected? Let’s unravel the mystery, one syllable at a time.
Defining the Lisp: More Than Just a Quirky Accent
A lisp is a speech sound disorder where someone struggles to articulate sibilant consonants like “s,” “z,” “sh,”* or *“ch.” Imagine your tongue as a conductor’s baton guiding airflow. In a lisp, the baton misses its mark, directing air sideways or against the teeth instead of smoothly over the tongue’s tip. This creates distorted sounds—think of it like a guitar string slightly out of tune.
Key Lisp Types:
1. Interdental Lisp (Frontal Lisp):
The tongue pushes between the front teeth, turning “sun” into “thun.”
Analogy: It’s like trying to drink from a straw with a hole—the airflow escapes where it shouldn’t.
2. Lateral Lisp:
Air slides over the tongue’s sides, creating a “slushy” or wet sound (e.g., “soup” sounds like “shoup”).
Comparison: Similar to water gurgling through a hose kink.
3. Palatal Lisp:
The tongue touches the soft palate, distorting sounds into something closer to “y” (e.g., “see” becomes “yee”).
Anecdote: Mark, a podcast host, spent years avoiding words like “statistics” due to his lateral lisp. After speech therapy, he now jokes, “My lisp didn’t stand a chance against my stubbornness!”
Why Do Lisps Happen? Unpacking the Causes
Developmental Factors (Common in Children):
Oral Motor Delays: Weak tongue or lip muscles can misdirect airflow.
Habitual Patterns: Prolonged thumb-sucking or pacifier use may train the tongue to rest incorrectly.
Genetic Links: While not directly inherited, family patterns of speech delays or dental structures (e.g., overbites) can play a role.
Metaphor: Speech development is like learning piano—missed practice or awkward hand placement leads to off-key notes.
Acquired Causes (Adults):
Dental Work or Injury: A new dental crown or jaw misalignment can temporarily alter speech.
Neurological Issues: Strokes, brain injuries, or conditions like Parkinson’s may affect muscle control.
Stress or Fatigue: Ever noticed slurred speech during exhaustion? Tension can mimic a lisp.
Example: After a car accident damaged her facial nerves, Clara developed a sudden interdental lisp. With therapy, she regained 90% of her clarity within a year.
“Can You Fix a Lisp?” Spoiler: Yes, and Here’s How
For Children:
Early Intervention (Ages 3-7):
Speech therapists use playful tools like mirrors, straw exercises, or games (e.g., “snake hisses” for “s” sounds).
Positive Reinforcement: Celebrate progress, even small wins!
Pro Tip: Turn practice into play. Pretend to be a snake (“ssss”) or a bee (“zzzz”) during bath time.
For Adults:
Speech Therapy: Techniques include:
Tongue Placement Drills: Practice resting the tongue tip behind the teeth.
Minimal Pairs: Differentiate similar words (e.g., “sip” vs. “ship”).
Recording Sessions: Hearing yourself improves self-awareness.
At-Home Exercises:
Straw Drinking: Sipping water through a straw strengthens tongue muscles.
“Silly Sentences”: Repeat tongue-twisters like “Sally sells seashells by the seashore.”
Anecdote: Jonathan, a lawyer, practiced his “s” sounds during commutes. “I’d mutter ‘supersedes’ 50 times a day. My Uber drivers thought I was nuts!”
Words That Trip Up Lispers (and How to Tackle Them)
Some words feel like verbal obstacle courses for those with lisps:
Hard Words to Say: “Statistics,” “squirrel,” “specific,” “exacerbate.”
Why? They combine multiple “s” or “sh” sounds with complex syllables.
Strategy: Break words into chunks. For “statistics,” practice “sta-ti-stics” slowly, then speed up.
FAQs: Your Top Lisp Questions, Answered
Are lisps genetic?”
While no “lisp gene” exists, inherited traits like jaw structure or family speech patterns can increase likelihood.
“Can stress cause a sudden lisp in adults?”
Yes! Tension tightens oral muscles, altering airflow. Relaxation exercises often help.
“Is a lisp a speech impediment?”
Technically, yes—but many view it as a difference, not a disability. Think of it like a regional accent.
“How long does it take to correct a lisp?”
Children: 3–6 months with consistent therapy. Adults: 6–12 months, depending on dedication.
Embracing Progress, Not Perfection
A lisp might feel like a roadblock, but it’s more like a detour—one that can lead to resilience and self-awareness. Take it from famous voices like actor Jonathan Ross or musician Sam Smith, who’ve turned their unique speech patterns into trademarks.
Final Thought: Your voice is more than its quirks. Whether you’re a parent guiding a child or an adult reclaiming clarity, every practiced “s” is a step toward confidence. After all, even the smoothest rivers have rocks—they just learn to flow around them.
Why Do Babies Drool So Much?
Drooling is a natural part of infancy, but when does it signal something more? Explore the science behind baby drool, practical management tips, and reassurance for parents navigating this slippery phase.
As a new parent, you’ve likely marvelled at your baby’s tiny fingers, their first smiles, and the soft sounds of their coos. But you’ve probably also noticed something less glamorous: drool. Pools of it. Whether your 2-month-old is suddenly salivating like a leaky faucet or your 3-month-old seems to be blowing bubbles nonstop, drooling is a universal (and messy) part of infancy. But why does it happen? When is it normal, and when should you worry? Let’s dive into the science, stories, and solutions behind baby drool.
The Science of Slobber: Why Do Babies Drool?
Imagine your baby’s mouth as a tiny, efficient factory. Saliva is its primary product—a natural lubricant that aids digestion protects gums, and even fights germs. But babies haven’t yet mastered the art of swallowing on command in the early months. Combine that with underdeveloped muscle control, and you’ve got a recipe for drool overflow.
Key Reasons Babies Drool:
1. Developmental Milestones: At 2-3 months, babies begin exploring their mouths with their tongues, a phase that often kickstarts drooling. Think of it as their first “science experiment” with body parts!
2. Teething Prep: Even before teeth emerge (around 6 months), saliva production ramps up to soothe tender gums.
3. Oral Exploration: Babies use their mouths to learn about textures, tastes, and cause-and-effects (like blowing raspberries!).
4. Digestion Support: Saliva helps break down milk or formula, priming their tiny stomachs for solids later.
Analogy Alert! Drooling is like a sprinkler system for your baby’s mouth—it keeps things moist, clean, and ready for growth.
Age-by-Age Drooling Guide: What’s Normal?
Newborns (0-1 Month):
Newborns typically don’t drool much since their salivary glands are still “warming up.” However, occasional drool bubbles are harmless. If your newborn is salivating excessively, check for feeding issues (like difficulty latching) and consult your pediatrician.
Anecdote: Sarah, a mom of twins, noticed her 3-week-old drooling during sleep. Her pediatrician reassured her it was normal—just a sign of her baby’s glands activating.
1-2 Months:
Around this age, babies start gaining head control and discovering their hands—cue the drool! A 2-month-old drooling a lot might simply be practicing tongue movements or reacting to increased saliva production.
Example: If your 2-month-old is drooling and blowing bubbles, they’re likely “talking” to you in their own adorable way.
3-4 Months:
By 3 months, drooling often peaks. Babies chew on fists, toys, or clothing to soothe gums (even if teeth are months away). A 3-month-old drooling a lot might also be preparing for teething or mastering new motor skills.
Metaphor: Teething prep is like a construction crew working behind the scenes—drool is the “debris” of growth!
6+ Months:
Once solids are introduced, drooling usually decreases as swallowing reflexes mature. However, teething can trigger temporary spikes.
When Drooling Becomes a Concern: Red Flags
While drooling is typically harmless, it can occasionally signal an issue:
Difficulty Breathing or Swallowing: Excessive drool paired with choking, gagging, or fever could indicate infection (e.g., hand-foot-and-mouth disease) or reflux.
Sudden Changes: A sudden increase in drooling in toddlers (e.g., a 2-year-old drooling) might relate to allergies, neurological conditions, or speech delays.
Persistent Drooling Beyond Toddlerhood: Most kids stop drooling by 18-24 months. If your 3-year-old is still drooling excessively, consult a speech therapist.
Comparison: Just as a car’s check engine light signals deeper issues, persistent drool and other symptoms warrant a professional “diagnostic scan.”
How to Manage the Drool Deluge: Practical Tips
For Infants (0-12 Months):
Bib Brigade: Soft, absorbent bibs are your best friend. Rotate them frequently to prevent rashes.
Teething Toys: Chill (not freeze) silicone toys to numb gums and reduce saliva flow.
Gentle Wiping: Use a soft cloth to dab—not rub—your baby’s chin. Over-wiping can irritate skin.
Hydration Check: Ensure your baby isn’t drooling due to thirst, especially in hot weather.
Pro Tip: For a 2-month-old drooling bubbles, snap a photo—it’s a phase you’ll laugh about later!
For Toddlers (1-3 Years):
Teach Swallowing: Play “swallow games” (e.g., pretending to gulp like a dinosaur) to build muscle memory.
Speech Practice: Excessive drooling in toddlers can sometimes link to speech delays. Singing or blowing bubbles strengthens oral muscles.
FAQs: Answering Your Top Drooling Questions
Why is my 2-month-old drooling so much?
At 2 months, drooling is often linked to developmental leaps (like discovering their tongue) or early teething prep. It’s rarely a concern unless paired with fussiness or fever.
When do babies stop drooling?
Most taper off by 18 months, but timing varies. My nephew, for instance, was a “drool champion” until his molars arrived at 15 months!
“Can I stop my baby from drooling?”
Drooling is natural—you can’t (and shouldn’t) stop it entirely. Focus on managing messes and protecting sensitive skin.
The Silver Lining in the Drool Cloud
Yes, drool stains on onesies and endless laundry can feel overwhelming. But remember: drooling is a sign your baby’s body is working exactly as it should. Each droplet is a tiny badge of growth, curiosity, and preparation for milestones like crawling, talking, and, eventually, eating ice cream without a bib.
Final Thought: Like rain nurturing a garden, drool nourishes your baby’s development. Grab those bibs, embrace the mess, and know this phase will pass—leaving you with hilarious stories and a heart full of memories.
Why Do Babies Stick Their Tongues Out?
Is your newborn sticking their tongue out constantly? Learn why this adorable habit is normal, how reflexes like tongue thrusting play a role, and when to seek guidance. Plus, tips for addressing tongue thrust in adults.
Few things are as endearing as watching a baby explore the world with their tiny tongue. Whether it’s a 2-month-old mimicking facial expression or a 9-month-old experimenting with new sounds, tongue protrusion is a common—and often misunderstood—behaviour. But why do babies stick their tongues out so much? Is it a reflex, a developmental phase, or a sign of something more?
This guide will explore the science behind tongue thrusting, the extrusion reflex, and how these behaviours evolve from infancy to adulthood. We’ll also share practical tips for parents and answer questions like “Why does my baby keep sticking her tongue out?” and “How do I stop tongue thrusting in older children or adults?”.
The Science Behind Baby Tongue Movements
1. Newborn Reflexes: The Extrusion and Tongue Thrust Reflex
When a newborn sticks their tongue out repeatedly, it’s often tied to two reflexes:
Extrusion Reflex:
This instinct helps babies latch during breastfeeding or bottle-feeding. If you gently touch a newborn’s lips, they’ll push their tongue forward (or “extrude”) to help draw milk. This reflex fades around 4–6 months.
Tongue Thrust Reflex:
A protective mechanism to prevent choking, this reflex causes babies to push food (or foreign objects) out of their mouths with their tongues. It’s why your 3-month-old might reject a pacifier by thrusting it out.
Example: A parent notices their 2-week-old sticking their tongue out after feeding. This is likely the extrusion reflex at work, ensuring the baby doesn’t overeat.
2. Developmental Exploration
Babies use their mouths to explore textures, tastes, and cause-and-effect. By 2–3 months, they may stick their tongue out to mimic caregivers or experiment with motor skills.
Anecdote: “My 3-month-old started copying me when I stuck my tongue out! It’s how she learns to communicate,” shares mom Jessica.
3. Teething and Oral Discomfort
At 6–9 months, teething can lead to excessive tongue movements. Babies might push their tongue against sore gums or drool more, making tongue protrusion more noticeable.
Age-by-Age Guide: What’s Normal?
Newborn to 2 Months
Normal: Frequent tongue thrusting during feeds, sticking tongue out after eating.
When to Ask: If the baby struggles to latch or seems frustrated during feeding.
2–6 Months
Normal: Mimicking faces, playful tongue sticking, reduced extrusion reflex.
Example: A 4-month-old sticks their tongue out when excited—no cause for concern.
6–12 Months
Normal: Teething-related tongue pushing, babbling with tongue movements.
When to Ask: If tongue thrusting interferes with eating solid foods.
Is It Tongue Thrust? Signs to Watch For
While most tongue protrusion is harmless, persistent tongue thrusting beyond infancy can affect speech, swallowing, or dental health.
Signs in Babies
Difficulty transitioning to solids (e.g., baby pushes food out with tongue at 9 months).
Chronic open-mouth posture (tongue always resting outside).
Signs of Tongue Thrust in Adults
Lisping or speech issues.
Tongue pressing against teeth when swallowing.
Dental problems (e.g., misaligned teeth).
Comparison:
Normal: A 2-month-old sticking their tongue out during play.
Concerning: A 3-year-old who still pushes food away with their tongue.
Addressing Tongue Thrust: Tips for Parents
For Infants
Practice Oral Motor Exercises: Gently rub gums or offer teething toys to strengthen mouth muscles.
Model Proper Swallowing: Show your baby how to close their lips while eating.
For Older Children and Adults
Tongue Thrust Therapy: Speech therapists use exercises to retrain tongue posture.
Myofunctional Therapy: Focuses on correcting swallowing patterns.
Success Story: “After six months of therapy, my daughter stopped thrusting her tongue, and her speech improved dramatically,” says dad Mark.
FAQs: Answering Your Top Questions
Q: Why does my baby stick her tongue out so much?
A: It’s usually exploration, imitation, or reflexes. At 2 months, it’s rarely a concern.
Q: How do I stop tongue thrusting in my child?
A: For babies, most outgrow it. For older kids, consult a speech therapist.
Q: Is tongue thrust linked to autism?
While developmental delays may affect oral motor skills, tongue protrusion alone isn’t a diagnosis. Always consult a pediatrician for evaluation.
Final Thoughts: Celebrate the Quirks
From a newborn’s tongue thrusting to a giggly 9-month-old’s antics, these behaviors are milestones in disguise. While staying informed is key, remember: that tiny tongue is just learning its way around a big world.
Need More Help? If tongue thrusting persists or affects daily life, reach out to a pediatrician or speech therapist. Early intervention can make all the difference!
DIY Throat Massage: Ease Throat Pain, Fatigue & MTD
From DIY throat massage techniques to navigating local specialists like ENTs near me or voice therapists near me, this comprehensive guide offers actionable solutions for throat pain, hoarseness, and vocal strain—plus tips to prioritize long-term vocal health.
We’ve all been there—waking up with a scratchy, sore throat that makes swallowing feel like a chore. While tea and lozenges are go-to remedies, natural techniques like massage for sore throat discomfort and professional care from an “ENT specialist near me” or “vocal therapist near me” can offer lasting relief. This guide will explore how to soothe throat pain, manage muscle tension dysphonia, and find the right experts near you.
Part 1: Understanding Throat Pain and Muscle Tension Dysphonia
What Causes Throat Pain?
Throat soreness can stem from infections (like strep), allergies, acid reflux, or overuse. However, muscle tension dysphonia (MTD)—a condition where vocal cords are strained due to tight neck and laryngeal muscles—is often overlooked. MTD is common among teachers, singers, and anyone who uses their voice excessively.
Key Symptoms of MTD:
Hoarseness or raspy voice
The sensation of a "lump" in the throat
Pain when speaking or swallowing
Fatigue after vocal use
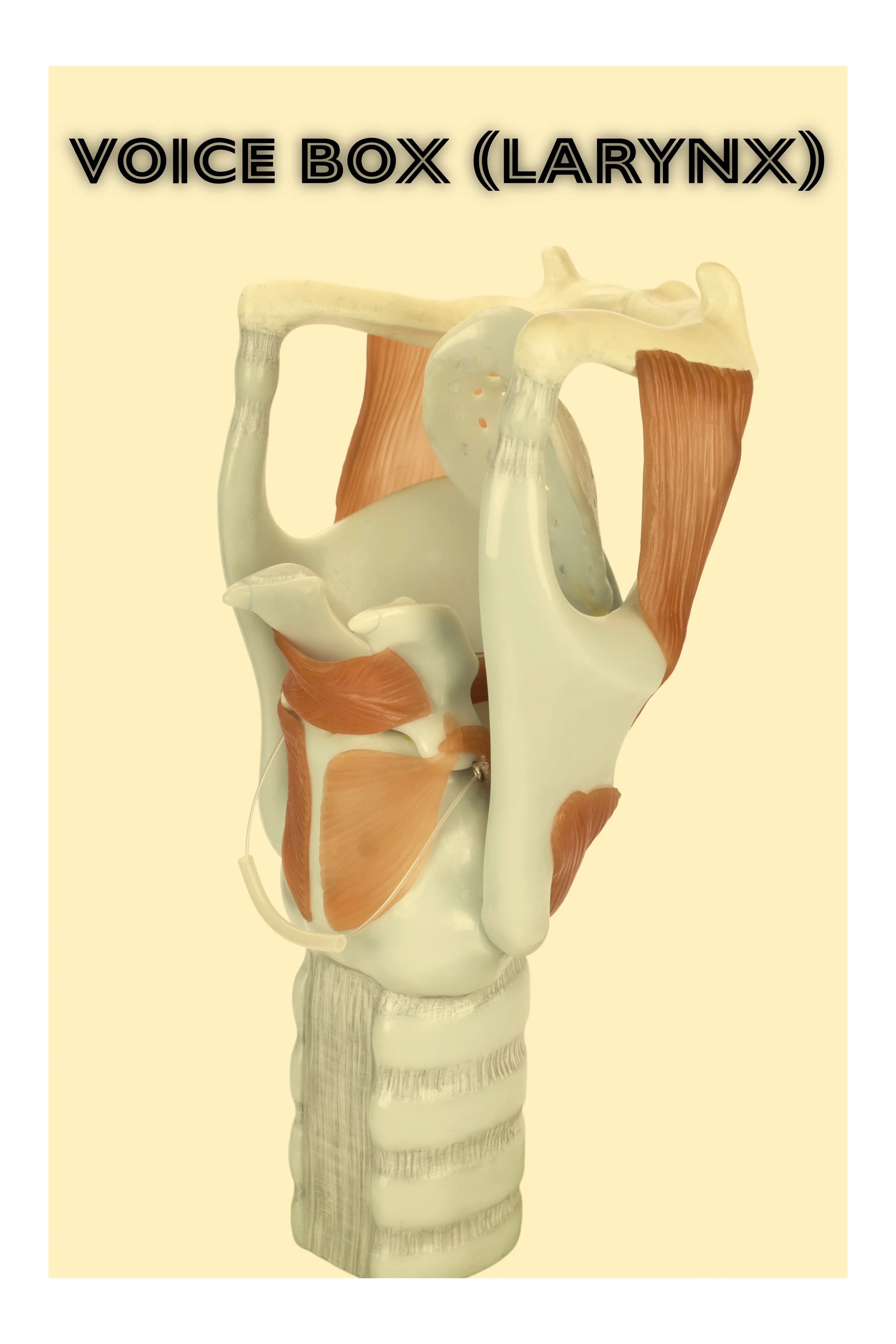
The Role of Throat Muscles in Vocal Health
Your larynx (voice box) is surrounded by intricate muscles that control pitch, volume, and airflow. When these muscles tighten due to stress, poor posture, or overuse, they can compress the vocal cords, leading to pain and voice changes. Think of it like a guitar string: too much tension creates a harsh, strained sound.
Part 2: Can Massaging a Sore Throat Help?
The Science Behind Throat Massage
Gentle laryngeal massage and circumlaryngeal massage target the muscles around the voice box to release tension. Studies show these techniques improve blood flow, reduce inflammation, and alleviate MTD symptoms. For example, a 2018 study in the Journal of Voice found that patients who combined massage with “voice therapy near me” sessions saw a 70% reduction in vocal strain.
How It Works:
1. Relaxes Muscles: Like kneading a tight knot in your shoulder, massage loosens hyperactive laryngeal muscles.
2. Improves Alignment: Reduces strain on vocal cords by correcting posture imbalances.
3. Enhances Hydration: Stimulates mucus membranes, preventing dryness.
Step-by-Step Guide to Throat Massage
Always consult a “vocal cord specialist near me” before trying new techniques.
1. Circumlaryngeal Massage:
Place your thumb and index finger on either side of your Adam’s apple.
Gently rock the larynx side-to-side for 2–3 minutes.
Finish with upward strokes along the neck to release tension.
2. Jaw and Neck Release:
Massage the base of your skull (where the neck meets the skull) in circular motions.
Open your jaw wide and gently stretch the muscles under the chin.
3. Steam + Massage Combo:
Inhale steam from a bowl of hot water (add eucalyptus oil for extra relief).
Follow with a gentle throat massage to loosen mucus and muscles.
Anecdote in Action:
Sarah, a teacher, struggled with chronic hoarseness until her “voice therapist near me” taught her DIY laryngeal massage steps. After weeks of practice, she noticed less strain during lectures and fewer sore throats.
Part 3: At-Home Exercises for Muscle Tension Dysphonia
Daily Routines to Reduce Vocal Strain
Pair throat massage with these exercises for muscle tension dysphonia:
1. Humming Scales
Hum a low-to-high pitch scale, focusing on smooth transitions.
Why it works: Engages vocal cords without strain.
2. Semi-Occluded Vocal Tract Exercises (SOVTEs)
Hum through a straw into a glass of water for 5 minutes.
Why it works: Balances airflow and reduces vocal cord impact.
3. Neck and Shoulder Stretches
Tilt your head side-to-side, holding each stretch for 15 seconds.
Roll shoulders backward to improve posture.
4. Diaphragmatic Breathing
Place a hand on your abdomen; inhale deeply through the nose, letting your belly rise.
Exhale slowly through pursed lips.
Pro Tip: Record your voice before and after exercises to track progress.
Part 4: When to Seek Professional Help
Red Flags: Symptoms That Need an Expert
While DIY care helps mild cases, consult a “throat specialist near me” if you experience:
Hoarseness lasting over 2 weeks
Painful swallowing or breathing
Unexplained weight loss
Ear pain or nasal congestion (see an “ear nose and throat doctor close to me”)
Types of Specialists to Consider
1. ENT (Otolaryngologist):
Treats structural issues like nodules, polyps, or reflux.
2. Laryngologist:
Subspecializes in voice disorders.
3. Speech-Language Pathologist (SLP):
Provides voice therapy near me for MTD.
4. Vocal Coach:
For singers needing technique adjustments.
Comparison: Just as you’d visit a sinus surgeon near me for chronic congestion, a “vocal cord specialist near me” addresses voice issues with tailored treatments like circumlaryngeal massage training or vocal therapy.
Part 5: Finding the Right Specialist Near You
How to Search Effectively
1. Use Precise Keywords:
“ENT near me within 5 mi”
“Speech pathologist voice specialist near me”
“ENT open on weekends near me”
2. Check Credentials:
Look for board certification in otolaryngology or speech pathology.
Read reviews for “high-rated ENT doctors” or “best throat doctors near me”.
3. Ask for Referrals:
Primary care doctors or choirs often know trusted voice specialists near me.
Case Study: Tom, a podcaster, ignored his chronic throat pain until a “voice doctor near me” diagnosed MTD. He regained his smooth, podcast-ready voice with “voice therapy near me” sessions and massage.
Part 6: The Role of Massage in Long-Term Vocal Health
Beyond Sore Throats: Holistic Benefits
Regular throat massage benefits include:
Stress Reduction:
Lowers cortisol levels, easing tension.
Improved Posture:
Releases neck muscles linked to slouching.
Vocal Clarity:
Ideal for singers, teachers, or public speakers.
Combining Massage with Other Therapies
Hydration:
Drink warm water with lemon to keep mucus thin.
Vocal Rest:
Avoid whispering (it strains cords more than speaking).
Humidifiers:
Add moisture to prevent dryness-induced irritation.
Pro Tip: Schedule a monthly “vocal therapist near me” session for maintenance, like a tune-up for your voice.
Part 7: Navigating Healthcare Systems and Insurance
What to Expect During Your First Visit
1. ENT Appointment:
A scope may be inserted through the nose to examine the larynx.
Tests for reflux, allergies, or infections.
2. Speech Therapy Evaluation:
Assessment of breathing, pitch, and speech habits.
Customized muscle tension dysphonia treatment at home plan.
Insurance Tips
Verify if your plan covers “speech therapy near me for adults” or “otolaryngology near me”.
Ask about sliding-scale fees at “ENT clinics near me” if uninsured. Canadian? Free care, but be prepared for a 6-12 month wait for an appointment
Part 8: Prevention and Long-Term Care
Daily Habits for a Healthy Throat
1. Stay Hydrated:
Aim for 8 glasses of water daily.
2. Avoid Strain:
Use a microphone for public speaking.
3. Practice Good Posture:
Align ears with shoulders to ease neck tension.
When to Schedule Check-Ups
Annual ENT Visit: Especially if you’re a vocal professional.
Post-Infection Follow-Up: After strep or laryngitis.
Final Thoughts
A sore throat might feel like a minor annoyance, but it’s your body’s way of saying, “Slow down!” Whether you’re practicing laryngeal massage steps or booking a “top-rated ENT near me”, proactive care keeps your voice resilient.
Ready to take action? Search “best ENT specialist near me” or “speech language pathologist near me” today—and give your throat the TLC it deserves!
FAQs
Q: How often should I massage my throat for soreness?
A: 2–3 times daily during acute pain; 3–4 times weekly for maintenance.
Q: Can stress cause muscle tension dysphonia?
A: Yes! Stress tightens throat muscles—pair massage with meditation or yoga.
Q: Are there free resources for vocal exercises?
A: Many “speech pathology near me” clinics offer free guides online.
Vocal Cord Paralysis vs. Paresis: Key Differences, Symptoms, and Treatments
When James, a podcast host, noticed his voice cracking mid-recording, he assumed it was overuse. But when his ENT mentioned **vocal cord paresis**—partial weakness of the vocal cords—he realized not all voice disorders are the same. Paralysis and paresis are often confused, yet their impact on speech, breathing, and quality of life varies dramatically. Let’s unravel their differences and uncover pathways to recovery.
When James, a podcast host, noticed his voice cracking mid-recording, he assumed it was overuse. But when his ENT mentioned vocal cord paresis—partial weakness of the vocal cords—he realized not all voice disorders are the same. Paralysis and paresis are often confused, yet their impact on speech, breathing, and quality of life varies dramatically. Let’s unravel their differences and uncover pathways to recovery.
Paralysis vs. Paresis: What’s the Difference?
Vocal Cord Paralysis
Definition: Complete loss of movement in one or both vocal cords.
ICD-10 Codes: Unilateral: J38.01, Bilateral: J38.02
Severity: Often linked to nerve damage (e.g., recurrent laryngeal nerve injury).
Vocal Cord Paresis
Definition: Partial weakness or reduced mobility of the vocal cords.
ICD-10 Code: J38.3 (vocal cord weakness, unspecified).
Severity: Less severe than paralysis but can progress if untreated.
Symptoms: How They Compare
Shared Symptoms
Hoarseness
Voice fatigue
Difficulty projecting speech
Unique to Vocal Cord Paralysis
1. Breathing Issues:
Bilateral vocal cord paralysis often causes stridor (high-pitched breathing) or airway obstruction.
Example: A newborn with bilateral vocal cord paralysis at birth may require a tracheostomy.
2. Severe Aspiration Risk: Weak cough reflex increases choking hazards.
Unique to Vocal Cord Paresis
1. Intermittent Symptoms: Voice may improve with rest.
2. Mild Airflow Issues: Rarely causes stridor but may lead to shortness of breath during exertion.
Case Study: Emily, a teacher with left vocal cord paresis, could speak clearly in the morning but lost her voice by afternoon. Therapy focused on reducing muscle strain.
Causes: From Nerve Damage to Infections
Vocal Cord Paralysis Causes
1. Surgery: Thyroidectomy (25-30% of cases).
2. Trauma: Neck injuries or prolonged intubation.
3. Neurological: Stroke, ALS, or COVID vocal cord paralysis (rare but documented).
Vocal Cord Paresis Causes
1. Overuse: Chronic voice strain (common in singers).
2. Neuropathy: Early-stage nerve compression (e.g., from acid reflux).
3. Idiopathic: No identifiable cause in 15-20% of cases.
Key Insight:
Paresis is often a precursor to paralysis. For instance, partial paralysis of the vocal cords might begin as paresis before nerves fully degrade.
Diagnosis: Imaging, Scopes, and Voice Analysis
Shared Diagnostic Tools
Laryngoscopy: Visualizes cord movement.
CT/MRI: Rules out tumours (e.g., vocal cord paralysis radiology).
Differentiating Tests
1. Electromyography (EMG):
Measures nerve activity.
Paresis shows reduced signals; paralysis shows none.
2. Flow Volume Loop:
Bilateral vocal cord paralysis creates a “fixed obstruction” pattern.
Paresis may show minor airflow irregularities.
Example: A patient with abductor paralysis of vocal cords (cords stuck closed) had a flat inspiratory flow loop, while paresis showed fluctuating waves.
Treatment: Tailoring Solutions to Severity
For Paralysis
1. Surgery:
Vocal cord paralysis surgery (e.g., thyroplasty, injection laryngoplasty).
Bilateral vocal cord paralysis treatment** may require cordectomy or tracheostomy.
2. Voice Therapy:
Post-surgery exercises with a Speech Pathologist to optimize function (vocal cord paralysis exercises PDF).
For Paresis
1. Voice Rest and Therapy:
Speech therapy for vocal cord paralysis/paresis focuses on reducing strain.
Techniques like “straw phonation” improve airflow.
2. Medications:
Steroids for inflammation.
Antivirals if linked to infections (e.g., Lyme disease).
Success Story: After vocal cord paralysis therapy, Mark transitioned from paresis to full mobility in 6 months.
Living with Paralysis vs. Paresis
Paralysis Challenges
Airway Management: Severe cases need tracheostomy.
Diet Modifications: Thickened liquids to prevent aspiration.
Paresis Adjustments
Voice Conservation: Amplification devices for professionals.
Lifestyle Tweaks: Avoiding caffeine (dries vocal cords).
Tip for Parents:
Feeding a baby with vocal cord paralysis requires specialized bottles; paresis may only need slower feeds.
FAQs: Your Top Questions Answered
Q: Can paresis become paralysis?
A: Yes, if underlying nerve damage progresses (e.g., untreated tumours).
Q: Is vocal cord paresis curable?
A: Often reversible with early intervention (e.g., vocal cord paralysis treatment, speech therapy).
Q: How are they coded differently?
A: Paralysis uses J38.0x; paresis falls under J38.3.
Final Thoughts
Understanding the line between paralysis and paresis empowers better care. While paralysis demands urgent, sometimes surgical action, paresis offers a window for preventive therapy. Whether you’re battling unilateral vocal cord paralysis or mild paresis, modern medicine and therapy can help you find your voice again.
Consult a Speech Pathologist or ENT specialist if you experience persistent hoarseness.
Navigating High Functioning ADHD in Women: From Diagnosis to Empowerment
Sophia, a Toronto-based lawyer, thrived in court but collapsed into tears at home. Her ADHD diagnosis at 35 explained years of mood swings, burnout, and hyperfocus cycles. Like many women, she masked symptoms until pregnancy forced her to confront ADHD. Discover how to identify high-functioning ADHD, manage medication during pregnancy, and thrive in a neurodivergent world—with insights for Canadian women.
The Masked Reality of High Functioning ADHD in Women
Why Women Go Undiagnosed
High-functioning ADHD in women often hides behind achievement. Consider Dr. Emily, a surgeon who memorized protocols flawlessly but forgot her daughter’s school play. Research shows that women tend to internalize struggles, fearing labels like "scatterbrained" or "overemotional." Key traits include:
Functional ADD: Outward competence masking internal chaos (e.g., flawless work presentations but a cluttered car).
ADHD Mood Swings: Rapid emotional shifts, from frustration to tearfulness, often mistaken for PMS.
Giftedness Overlap: Twice-gifted ADHD (high IQ + executive dysfunction) leading to burnout.
Comparison: ADHD vs. giftedness: Both crave stimulation, but ADHD impairs task completion despite intelligence.
After earning her PhD, Maria failed to file paperwork for graduation—a classic "high functioning" gap.
Functional ADD vs. ADHD: Breaking Down Terminology
"Functional ADD" isn’t a medical term but describes individuals compensating for symptoms. Imagine ADHD as a smartphone with a drained battery: functional but inefficient.
Key Differences:
Hyperactivity: Less obvious in women (e.g., mental restlessness vs. physical fidgeting).
Emotional Dysregulation: ADHD mood swings (e.g., rage over misplaced keys) vs. situational stress.
Canadian Context: 60% of women with ADHD are misdiagnosed with anxiety or depression first (CAMH, 2023).
ADHD and Pregnancy: Medication, Risks, and Alternatives
Vyvanse During Pregnancy: A Canadian Perspective
An Ottawa engineer, Lena faced a dilemma: continue Vyvanse while pregnant or risk career-derailing focus loss. Her psychiatrist explained:
Vyvanse and other stimulant medications may have pregnancy risks: Limited data; potential low birth weight vs. maternal mental health risks.
ADHD Meds and Pregnancy Alternatives: Omega-3 supplements, CBT, and workplace accommodations.
Canadian Guidelines:
OHIP Coverage: ADHD testing is covered only if referred by a GP; private clinics cost $1,500-$3,000.
Postpartum Support: Post-ADHD medication titration may require re-assessment.
Non-Medication Strategies:
Time Management Apps: Focus@Will for ADHD-friendly productivity.
Delegation: Partner handles bills; virtual assistants manage schedules.
Self-Assessment Tools: Female ADHD Tests and Quizzes
Free Female ADHD Test Options
1. CADDRA Adult ADHD Self-Report Scale: Free download for Canadian residents.
2. "Do I Have ADHD Quiz Female": Online tools like ADDitude Magazine’s symptom checker.
3. ADHD in Women Checklist: Includes 15 markers (e.g., rejection sensitivity, hyperfocus on hobbies).
Caution: Self-tests like the "female ADHD quiz free" tools are screening aids, not diagnoses.
Canadian Pathway to Diagnosis:
1. Family Doctors: Can diagnose ADHD in BC and Ontario if trained.
2. ADHD Specialists Near Me: Search CADDAC’s directory for clinics in Toronto, Vancouver, etc.
3. Online ADHD Diagnosis Canada: Platforms like Frida offer assessments in 2-3 hours.
After a "female ADHD test free" quiz hinted at ADHD, Jasmin visited an "ADHD clinic near me" in Montreal, leading to a formal diagnosis.
The 7 Subtypes of ADHD: From Anxious ADD to Ring of Fire
Dr. Daniel Amen’s ADHD subtypes explain why one-size-fits-all treatments fail:
1. Classic ADD: Hyperactivity, distractibility.
2. Inattentive ADD: Daydreaming, sluggishness.
3. Overfocused ADD: Obsessive thoughts, rigidity.
4. Temporal Lobe ADD: Mood instability, memory lapses.
5. Limbic ADD: Chronic sadness, low energy.
6. Ring of Fire ADD: Sensory overload, irritability (brain scans show "ring" of hyperactivity).
7. Anxious ADD: Perfectionism, nervousness.
Temporal lobe ADHD vs. bipolar disorder: Both involve mood swings, but ADHD lacks manic episodes.
Case Study: Emma, with "anxious ADD," thrived on Strattera + yoga, avoiding stimulants that worsened anxiety.
The ADHD Brain: Scans, Structures, and Differences
ADHD Brain vs. Normal Brain: What Imaging Shows
Frontal Lobe: Underactive in ADHD, impairing planning (explains procrastination).
Basal Ganglia: Smaller, reducing dopamine transmission (ties to motivation struggles).
Default Mode Network: Overactive, causing daydreaming.
A neurotypical brain is a symphony; an ADHD brain is jazz—improvised but brilliant.
Neurodiversity in the Workplace: Thriving with ADHD
ADHD Workplace Accommodations Canada
Under the Accessibility for Ontarians with Disabilities Act (AODA), employers must provide:
Noise-cancelling headphones for sensory sensitivity.
Flexible deadlines for "hyperfocus slump" days.
Written instructions to counter working memory gaps.
Success Story: A Calgary tech firm saw a 30% productivity boost after allowing ADHD employees to work 11 AM–7 PM.
Remote Work Tips:
Use Toggl for time blindness.
Schedule "body doubles" (virtual coworking) for accountability.
ADHD and Relationships: Love, Conflict, and Communication
Dating Someone with ADHD: What to Expect
Strengths: Spontaneity, humor, hyperfocus on partners.
Challenges: Forgotten anniversaries, emotional dysregulation.
Strategies:
ADHD Partnership Contracts: Agree on chores (e.g., "I handle laundry; you manage finances").
Non-Medication Tools: Shared Google Calendars with reminders.
After fights over missed dates, Priya and her partner used Finch app check-ins to rebuild trust.
ADHD, Anxiety, and Depression: Untangling the Web
Does ADHD Cause Anxiety?
Yes—chronic underperformance fuels worry. A 2022 study found 47% of ADHD adults have generalized anxiety.
Treatment Options:
ADHD and Anxiety Meds:
Wellbutrin (dual-action for ADHD + depression).
Zoloft and ADHD: Can calm anxiety and depression but may worsen focus.
Canadian Mental Health Comorbidities: 32% of ADHD adults in Ontario have attempted suicide (CAMH, 2021).
Managing ADHD Without Medication: 12 Evidence-Based Strategies
Non-Drug Treatment for ADHD
1. Neurofeedback: Trains brainwaves; 60% efficacy per CADDAC.
2. Diet: High-protein breakfasts, omega-3s (salmon, walnuts).
3. Exercise: 30 minutes of cardio boosts dopamine, similar to Ritalin.
4. Sleep Hygiene: Weighted blankets combat ADHD insomnia.
Parent Tip: For "how to help a child with ADHD without medication," try martial arts for focus + discipline.
Canadian ADHD Resources: From Diagnosis to Tax Credits
How to Get ADHD Medication in Canada
1. Prescriptions: "ADHD doctors near me" can prescribe; online services like Ahead require a diagnosis.
2. Costs: Vyvanse costs $150/month in Canada; generic Adderall XR is $75.
3. Disability Tax Credit Canada: Apply via Form T2201 if ADHD severely impacts daily living
Provincial Differences:
Alberta: AISH funding may cover ADHD coaching.
BC: MSP partially covers psychologist assessments.
Final Checklist: Thriving with ADHD in Canada
1. Take a "female ADHD test free" if you suspect symptoms.
2. Consult an "ADHD specialist near me" for diagnosis.
3. Explore "non-drug treatment for ADHD” if avoiding meds.
4. Apply for "ADHD disability tax credit Canada" if eligible.
Navigating Sound Processing Challenges in Adulthood: Strategies and Insights
Have you ever struggled to follow conversations in noisy rooms or felt overwhelmed by rapid speech? For adults with Central Auditory Processing Disorder (CAPD), these challenges are daily realities. Dive into this guide to uncover symptoms, diagnosis, and actionable strategies for managing CAPD.
Imagine sitting in a busy café, trying to focus on a friend’s story while clattering dishes and overlapping conversations bombard your ears. For adults with auditory processing differences, this common scenario can feel overwhelming—not because their hearing fails, but because their brain struggles to filter and interpret sounds effectively. Let’s explore this invisible challenge, its links to auditory memory, head injuries, and practical solutions for daily life.
When Listening Feels Like Work: The Adult Reality
Sarah, a 34-year-old graphic designer, excels in her quiet studio but finds team meetings exhausting. "People assumed I wasn’t paying attention," she shares. "Truthfully, my brain couldn’t keep up with rapid conversations." After years of frustration, Sarah learned she had an auditory processing difference—a condition where the brain misinterprets sound signals despite normal hearing.
Her experience mirrors that of millions. Adults with auditory processing disorder (APD) often develop clever coping strategies but face daily hurdles in understanding speech, recalling verbal details, and managing sensory overload.
How Sound Processing Works (And When It Doesn’t)
Your ears detect sounds like a high-quality microphone, but the real work happens in your brain’s auditory cortex. Here’s where challenges emerge:
Sound Sorting: Struggling to prioritize voices over background noise
Auditory Memory: Difficulty retaining spoken instructions or conversation threads
Speed Processing: Needing extra time to decode rapid speech
Sound Blending: Hearing "fun ride" as "sunrise," especially post-head injuries
"Think of it like a smartphone with perfect hardware but buggy software," explains Dr. Linda Carter, an audiologist. "The sound input is clear, but the processing falters."
Spotting the Signs: Beyond "Bad Listening"
Adults with APD often hear the question, "Are you even listening?" when they’re trying extra hard to focus. Key indicators include:
📌 Frequent misunderstandings in noisy places
📌 Avoiding phone calls due to comprehension struggles
📌 Mental fatigue after conversations
📌 Reliance on lip-reading or written notes
📌 History of head injuries impacting sound processing
John, a high school teacher, recalls: "Staff meetings left me drained. I’d smile and nod, then realize I missed key details. My colleagues thought I was disengaged."
Why It Happens: Causes and Contributors
While research continues, several factors influence auditory processing challenges:
1. Neurological Wiring: Genetic differences in brain pathways
2. Head Trauma: Concussions or injuries affecting auditory regions
3. Early Infections: Chronic childhood ear issues altering development
4. Aging: Natural cognitive changes intensifying existing mild issues
5. Coexisting Conditions: Links to ADHD, autism, or learning differences
A 2022 *Journal of Auditory Research* study found that 68% of adults with APD reported previous head injuries, highlighting this often-overlooked connection.
Getting Answers: The Diagnosis Pathway
Step 1: Ruling Out Hearing Loss
A standard hearing test confirms physical ear health—usually normal in APD cases.
Step 2: Specialized APD Testing
Audiologists use tailored assessments like:
Speech-in-Noise Tests: Measuring comprehension amid background chatter
Temporal Processing Tasks: Assessing sound timing interpretation
Binaural Integration: Testing dual-ear sound combining
"Many adults cry during testing—not from pain, but relief," notes Dr. Carter. "Finally, their struggles make sense."
Life Hacks for Daily Success
Communication Strategies
The 3-Second Rule: Pause before responding to allow processing time
Visual Anchors: Pair verbal info with gestures or written keywords
Strategic Positioning: Sit facing speakers in meetings or gatherings
Tech Supports
Live Transcription Apps: Otter.ai or Google Live Caption
Directional Mics: Focus on specific speakers in noisy rooms
Custom Earplugs: Musician-style filters reducing overwhelm
Workplace Adaptations
Request written meeting summaries
Use noise-dampening headphones in open offices
Advocate for agenda-sharing before calls
Auditory Memory Boosters
Since APD often affects short-term sound retention, try these evidence-based exercises:
1. The Grocery List Game: Have someone dictate 5 items—recall them backwards
2. Podcast Paraphrasing: Listen to 3-minute segments, then summarize aloud
3. Lyric Learning: Memorize song verses through repeated listening
"Improved auditory memory helps me follow client calls better," shares Emma, a realtor with APD.
When APD Coexists with Other Conditions
APD & ADHD: Similar Symptoms, Different Roots
ADHD: Distraction from internal thoughts
APD: Distraction from sound misinterpretation
"Medication helps my focus," says software developer Tom, "but noise-filtering apps help me actually *hear*."
APD & Head Injury Recovery
Post-concussion patients often develop temporary processing issues. Targeted auditory therapy can aid neural repair.
Success in Action: Real Adult Wins
Case 1: The Restaurant Manager
After his APD diagnosis, Marco:
Installed sound-absorbing panels in his busy kitchen
Trained staff to use hand signals during loud rushes
Uses bone-conduction headphones for clearer communication
Case 2: The College Student
Lena accesses:
Lecture transcriptions via disability services
Extended test-taking time for auditory-heavy exams
Peer note-sharing through campus support programs
Hope in Progress: Emerging Research
1. Neuroplasticity Training: Apps rewiring brain sound processing
2. Biomarker Studies: Blood tests identifying APD subtypes
3. Gene Therapy Trials: Early-stage interventions for inherited forms
Taking Control: Your Action Plan
1. Connect: Find audiologists via the Canadian Academy of Audiology
2. Experiment: Try free apps like SoundSkills for basic training
3. Advocate: Share APD explainers with employers/friends
4. Track: Note situations causing most strain—target solutions there
"Understanding my APD didn’t fix everything," Sarah reflects, "but it gave me power. Now I ask for repeats without shame and take listening breaks when needed. I’m still me—just with better tools."
This journey isn’t about "fixing" how you process sound, but building environments where your brain thrives. With evolving research and growing awareness, adults with auditory processing differences are rewriting what’s possible—one conversation at a time.
*For further resources:*
Canadian Academy of Audiology (www.caa-aca.ca)
APD Support Groups on Meetup
"Living with APD" Webinar Series (free access through most libraries)
Silent Reflux: The Sneaky Sibling of Heartburn You Might Be Missing
Silent reflux (LPR) isn’t your typical acid reflux. Instead of heartburn, it disguises itself as a chronic sore throat, raspy voice, or that "lump in your throat" feeling. Discover how to differentiate it from GERD, why antacids like Tums often fall short, and actionable diet and lifestyle tips to soothe irritation, protect your vocal cords, and prevent long-term damage.
Imagine this: You’re a teacher who loves their job, but lately, your voice has been raspy and unreliable. You’re sipping tea, avoiding caffeine, and resting your vocal cords, but the hoarseness won’t quit. Or maybe you’re a foodie who’s developed a nagging sore throat that feels like a perpetual campfire in your neck. You’ve tried lozenges and hydration, but relief is fleeting. What’s going on? The culprit might not be a cold, allergies, or overuse of your voice—it could be silent reflux, a lesser-known but surprisingly common condition that often flies under the radar.
Let’s unpack what silent reflux is, how it’s different from the classic heartburn or GERD (gastroesophageal reflux disease) you’ve heard about, and why it’s so easy to overlook. Along the way, we’ll explore practical tips to manage symptoms, protect your vocal cords, and even enjoy meals without fear.
Silent Reflux vs. Common Reflux: What’s the Difference?
When most people think of acid reflux, they picture fiery heartburn creeping up the chest after a spicy meal or lying down too soon after eating. That’s classic GERD, where stomach acid flows backward into the esophagus, irritating its lining. But silent reflux—officially called laryngopharyngeal reflux (LPR)—is its subtler, sneakier cousin. Instead of burning your chest, the acid (and digestive enzymes like pepsin) travels higher, reaching your throat, vocal cords, and even the back of your nasal passage.
Key Differences at a Glance:
Classic GERD
Heartburn, regurgitation
Worse after eating/lying down
Esophageal irritation
Relieved by antacids like Tums or Pepto Bismol and lifestyle change
Silent Reflux (LPR)
Sore throat, hoarse voice
Chronic cough, "lump" feeling in throat (Globus)
Vocal cord damage, laryngitis
Relieved by proton-pump inhibitors or H2 blockers
The biggest distinction? Silent reflux often lacks the hallmark burning throat or chest discomfort. Instead, it masquerades as ENT (ear, nose, throat) issues, leaving people confused and undiagnosed for months—or even years.
Why Silent Reflux is So Sneaky (and Harmful)
Stomach acid is corrosive, but your esophagus has some defence mechanisms. However, your throat and vocal cords aren’t built to handle acid exposure. Over time, even small amounts of reflux can cause inflammation, scarring, or ulcers in delicate tissues.
Take Sarah, a podcast host who blamed her raspy voice on “overworking” during recording sessions. After weeks of voice rest with no improvement, an ENT specialist spotted redness and swelling near her vocal cords—a classic sign of LPR. “I never felt heartburn,” she said. “But my throat always felt scratchy, like I was getting sick.”
Silent reflux is also stealthy because symptoms can take hours to appear after eating. Acid might creep up while you’re sleeping, leading to morning hoarseness or a bitter taste in your mouth.
The Unusual Suspects: What Triggers Silent Reflux?
The same factors that worsen GERD—like fatty foods, caffeine, or tight clothing—can also fuel LPR. But silent reflux has unique triggers:
Weak upper esophageal sphincter: This “valve” at the top of your esophagus may not close properly, allowing acid to reach the throat.
Pepsin: This digestive enzyme, activated by acid, can linger in throat tissues and cause **inflammation** even after acid is neutralized.
Lifestyle habits: Singing, frequent talking, or breathing through your mouth (common in athletes or people with allergies) can dry out the throat, making it more vulnerable to irritation.
Even medications like beta-blockers (used for high blood pressure) can indirectly contribute by relaxing muscles that keep acid contained.
“But I’m Taking Tums!” Why OTC Meds Aren’t Always Enough?”
Antacids like Tums or Pepto Bismol neutralize stomach acid, offering quick relief for classic heartburn. However, silent reflux often requires a different approach. Since pepsin (not just acid) irritates the throat, lowering acid production with PPIs (proton pump inhibitors) or H2 blockers may be more effective in the long term.
That said, medication alone won’t solve the problem. Diet and lifestyle changes are critical.
Eating for Relief: A Diet for Reflux That Doesn’t Sacrifice Flavor
The goal isn’t to eliminate acid but to reduce stomach acid triggers and avoid foods that loosen the esophageal sphincter. Here’s how:
Skip the Usual Offenders: Citrus, tomatoes, chocolate, alcohol, and caffeine.
Embrace Alkaline Foods: Bananas, oatmeal, leafy greens, and almond milk can soothe irritated tissues.
Get Creative: Love pasta? Swap tomato sauce for a basil-avocado “pesto” (without garlic or lemon).
Sample Meal Idea:
Breakfast: Oatmeal with almond butter and sliced banana.
Lunch: Grilled chicken salad with avocado, cucumber, and olive oil.
Dinner: Salmon with steamed broccoli and quinoa.
Smaller, frequent meals also help prevent overfilling the stomach, reducing pressure on the sphincter.
Protecting Your Voice: Why Vocal Cords Deserve Extra TLC
Chronic silent reflux can lead to vocal cord damage, including nodules or ulcers. If your livelihood depends on your voice (teachers, singers, coaches), proactive care is essential:
Stay hydrated to keep mucus thin and protective.
Avoid whispering, which strains the voice more than speaking softly.
Use a humidifier at night to combat dryness from nighttime reflux.
The Bottom Line: Don’t Ignore the Subtle Signs
Silent reflux thrives on being misunderstood. If you’ve been battling a stubborn sore throat, hoarseness, or that annoying Globus sensation, consider LPR as a possible cause. Track your symptoms, experiment with a diet for reflux, and consult a gastroenterologist or ENT specialist. With the right mix of medication, dietary tweaks, and vocal care, you can extinguish that silent burn and reclaim your comfort and voice.
Tongue Thrust: How It Impacts Speech, Teeth, and Effective Treatment Options
Tongue thrust is a common but often overlooked condition that can alter speech, cause misaligned teeth, and disrupt swallowing. This guide explores its effects and offers actionable solutions to restore oral health.
Imagine this: A bright-eyed 8-year-old named Emma loves telling stories, but her words often come out mumbled or slurred. Her parents notice her front teeth are splayed outward, creating a gap. After visits to a speech therapist and orthodontist, they learn Emma has *tongue thrust*—a habit of pushing her tongue against her teeth when speaking or swallowing. Like Emma, millions of people unknowingly live with this condition, which can subtly reshape their smiles, speech, and confidence.
In this post, we’ll explore how tongue thrust impacts daily life, its long-term effects on dentition, and the treatments that can correct it—whether you’re a parent, an adult, or simply curious about oral health.
What Is Tongue Thrust?
Tongue thrust (tongue pushing) occurs when the tongue presses too forcefully against the teeth during swallowing, speaking, or at rest. While infants naturally use this motion to suckle, most children outgrow it by age 6. When it persists, it becomes an oral habit with far-reaching consequences.
A Quick Comparison:
Think of tongue thrust like constantly leaning on a fence. Over time, the fence (your teeth) bends out of place. Similarly, repeated pressure from the tongue can shift teeth, alter jaw alignment, and even affect facial structure.
How Tongue Thrust Impacts Speech and Dentition
1. Speech Challenges
When the tongue pushes against the teeth during speech, it distorts sounds like *“s,” “z,” “t,”* and *“d.”* For example, the word “sun” might sound like “thun.” This pattern, called a *lisp*, is a hallmark of tongue thrust.
James, a 30-year-old teacher, struggled with pronunciation for years. He avoided public speaking until a speech therapist identified his tongue thrust. He learned to reposition his tongue through exercises, transforming his clarity and confidence.
2. Dental Misalignment
Chronic tongue thrusting exerts constant pressure on teeth, often leading to:
Open Bite: Front teeth don’t touch when the mouth is closed.
Overjet: Upper teeth protrude outward (“buck teeth”).
Crowding: Teeth shift into crooked or misaligned positions.
Example:
Sarah, a teenager, underwent braces to fix her overjet, only to relapse post-treatment because her untreated tongue thrust pushed her teeth back.
Swallowing Dysfunction
A proper swallow involves the tongue pressing against the roof of the mouth. With tongue thrust, the tongue pushes forward, straining facial muscles and contributing to orthodontic issues.
Who’s at Risk?
Tongue thrust often develops alongside:
Prolonged thumb-sucking or pacifier use
Allergies/chronic nasal congestion (promoting mouth breathing)
Genetic factors like tongue size or jaw structure
Comparison:
Like thumb-sucking, tongue thrust is a “parafunctional” habit that interferes with normal oral function. However, its effects are more insidious because it’s harder to detect.
Effective Treatments for Tongue Thrust
The good news? Tongue thrust is treatable at any age. Solutions often combine speech therapy, orthodontics, and collaboration between specialists.
1. Myofunctional Therapy
This “physical therapy for the mouth” retrains the tongue’s posture and swallowing pattern. Exercises might include:
Practicing proper tongue placement (tip against the roof of the mouth)
Strengthening tongue muscles with resistance techniques
Using mirrors or apps for real-time feedback
Success Story:
After 12 weeks of therapy, Emma learned to swallow correctly. Her speech improved, and her orthodontist noted less pressure on her emerging adult teeth.
2. Orthodontic Treatment
Braces or aligners can correct misaligned teeth, but they’re most effective *after* addressing the underlying tongue thrust. Otherwise, relapse is likely.
Example:
Clear aligners with “tongue cribs” (a small wire barrier behind the teeth) prevent the tongue from pushing forward, protecting straightened teeth.
3. Habit-Breaking Appliances
Devices like palatal cribs or tongue trainers physically remind the tongue to stay in place. They’re often used alongside therapy for children.
4. Surgical Intervention (Rare Cases)
For severe structural issues (e.g., enlarged tonsils or a misaligned jaw), surgery may be recommended to improve airway space or tongue function.
Early Intervention Matters
Children as young as 4 can benefit from screening. Adults, too, see results—though treatment may take longer.
Comparison:
Correcting tongue thrust is like fixing posture: The earlier you start, the easier it is to retrain muscle memory. But even adults can relearn healthier patterns with patience.
Final Thoughts: Don’t Ignore the Signs
Tongue thrust isn’t just a “bad habit.” Left unchecked, it can lead to costly dental work, self-consciousness, or even sleep apnea. If you notice:
Frequent lisps or speech errors
Protruding or spaced teeth
Mouth breathing or chewing difficulties
…consult a dentist, orthodontist, or myofunctional therapist, or speech pathologist. With the right approach, a healthier smile—and clearer speech—are within reach.
Worried about tongue thrust? Share this post with a friend, or book a consultation with an oral health professional today. Small changes today can prevent big problems tomorrow.
Embracing Fluency: How MBCT Can Support Those Who Stutter and Clutter
Stuttering and cluttering can feel isolating, but Mindfulness-Based Cognitive Therapy (MBCT) offers a path to reclaim confidence. By blending mindfulness practices with cognitive reframing, MBCT helps reduce speech-related anxiety, challenge negative self-talk, and embrace self-compassion. Dive into practical tips, relatable anecdotes, and insights on how this approach complements traditional speech therapy to empower your voice.
Introduction: The Struggle with Speech
Imagine standing in front of a room full of colleagues, your heart racing as you prepare to speak. You know your ideas are valuable, but the words feel trapped, tangled by stuttering or rushing out in a disorganized cluttered mess. This scenario is all too familiar for millions of people who stutter or clutter. Speech disruptions can lead to frustration, social anxiety, and self-doubt. But what if there was a way to reframe this struggle—not by eliminating it, but by changing your relationship with it? Enter *Mindfulness-Based Cognitive Therapy (MBCT)*, a compassionate, evidence-based approach that’s showing promise in helping individuals manage the emotional and cognitive challenges tied to speech differences.
What is MBCT? A Brief Primer
MBCT blends the grounding principles of mindfulness—non-judgmental awareness of the present moment—with cognitive behavioural techniques that address unhelpful thought patterns. Originally developed to prevent depression relapse, MBCT has since been adapted for anxiety, chronic pain, and stress. At its core, MBCT teaches individuals to observe their thoughts and feelings without criticism, creating space to respond thoughtfully rather than react impulsively.
Stuttering, Cluttering, and the Role of Mindfulness
Stuttering involves interruptions in speech flow (repetitions, blocks, or prolongations), while *cluttering* is characterized by rapid, irregular speech that often sacrifices clarity for speed. Both can lead to avoidance of speaking situations and negative self-perception. Here’s how MBCT can help:
1. Reducing Anxiety’s Grip
Fear of judgment often exacerbates speech challenges. MBCT’s mindfulness practices, like breath awareness and body scans, help calm the nervous system. For example, *John*, a graphic designer who stutters, uses a “mindful pause” before meetings: He takes three deep breaths, notices the sensations in his chest, and reminds himself, “It’s okay to speak at my own pace.” This ritual reduces his pre-speech anxiety, making blocks feel less overwhelming.
2. Reframing Negative Thoughts
Cognitive therapy components of MBCT challenge beliefs like “My stutter makes me incompetent” or “No one will listen to me.” Individuals gain perspective by recognizing these thoughts as mental events—not facts. *Sarah*, a teacher who clutters, once believed her rapid speech made her seem “scatterbrained.” MBCT taught her to replace self-criticism with curiosity: “My thoughts are moving fast today. Let me slow down and anchor to my breath.”
3. Building Self-Compassion
Mindfulness encourages kindness toward oneself. A 2019 *Journal of Fluency Disorders* study found that self-compassion practices reduced shame in adults who stutter. Imagine treating yourself with the same patience you’d offer a friend struggling to communicate—that’s the shift MBCT fosters.
MBCT in Action: Real-Life Applications
Mindful Speaking Exercises: Practice grounding techniques (e.g., feeling your feet on the floor) before a conversation. This anchors you in the present, reducing the urge to rush.
Thought Labeling: When negative thoughts arise (e.g., “I’ll mess up”), silently note, “That’s a worry,” and return your focus to your breath or the listener’s face.
Post-Speech Reflection: After a social interaction, journal without judgment. Instead of “I failed,” try, “I felt tense, but I shared my idea. That took courage.”
Comparison to Traditional Approaches
Traditional speech therapy often focuses on techniques like connected speech or pacing, which are invaluable for improving fluency. However, MBCT complements these methods by addressing the emotional loop—anxiety about stuttering/cluttering leading to more tension, which worsens symptoms. Think of it as training both the body *and* mind: While speech therapists provide the tools, MBCT helps you wield them with greater calm and confidence.
Similarly, compared to standard Cognitive Behavioral Therapy (CBT), MBCT places heavier emphasis on mindfulness meditation. Where CBT might focus on restructuring thoughts logically, MBCT encourages observing them with detachment. For someone who stutters, this could mean acknowledging “I’m having a tough day” without spiralling into catastrophizing.
Practical Tips to Get Started
1. Begin with Breath: Spend 5 minutes daily focusing on your breath. When your mind wanders to speech-related worries, gently guide it back.
2. Body Scan Meditation: Notice areas of tension (jaw, shoulders) linked to speech anxiety. Soften them intentionally.
3. Mindful Listening: In conversations, focus fully on the speaker. This shifts attention away from self-monitoring and reduces pressure.
4. Join a Group: Many MBCT programs offer group sessions, fostering connection and normalizing struggles.
Conclusion: A Journey of Acceptance, Not Perfection
MBCT isn’t about erasing stuttering or cluttering—it’s about transforming your response to them. Like learning to dance in the rain rather than waiting for the storm to pass, mindfulness invites you to find steadiness amid life’s unpredictability. Progress might look like speaking up more often, feeling less shame after a disfluent moment, or simply greeting your thoughts with a little more kindness.
If you’re navigating speech challenges, remember: Your voice matters for its fluency and the unique perspective it brings. MBCT is one tool to help you share it with the world—one mindful breath at a time.
Chris Dunphy is a speech-language pathologist and mindfulness advocate who is passionate about empowering individuals to communicate confidently. When not writing or coaching, he can be found singing karaoke with reckless abandon.
Mindfulness-Based Cognitive Therapy (MBCT) for Voice and Speech Disorders
Struggling with a hoarse, strained, or unreliable voice? Discover how Mindfulness-Based Cognitive Therapy (MBCT) bridges the gap between mind and body to treat voice disorders. From podcasters to teachers, learn how real people found relief—and how you can too—with science-backed strategies, lighthearted anecdotes, and a dash of humour.
Picture this: You’re about to give a presentation at work. Your throat feels tight, your voice cracks like a teenager’s mid-growth spurt, and suddenly, you sound less like a confident professional and more like Kermit the Frog after a night of karaoke. For many people, voice disorders aren’t just a fleeting inconvenience—they’re a daily battle that impacts careers, relationships, and self-esteem. Enter Mindfulness-Based Cognitive Therapy (MBCT), a gentle yet powerful approach that’s gaining traction not just for mental health but for treating voice disorders, too. Let’s explore how tuning into the present moment might help you reclaim your voice—literally.
The Symphony of Stress and Voice: A Modern Dilemma
Voice disorders—think chronic hoarseness, muscle tension dysphonia, or even psychogenic voice loss—often stem from a perfect storm of physical strain and emotional turbulence. Stress, anxiety, and negative thought patterns can turn our vocal cords into tight guitar strings, producing shaky notes instead of smooth melodies.
Take Sarah, a podcast host who suddenly developed a raspy, unreliable voice during a high-stakes season of her career. Doctors found no physical cause, but her SLP noticed her shoulders were perpetually hunched “like a turtle hiding from life.” Sarah’s voice wasn’t broken—it was *burdened*. That’s where MBCT comes in.
What Is Mindfulness-Based Cognitive Therapy? (And Why Should You Care?)
MBCT is like the lovechild of ancient mindfulness practices and modern cognitive therapy. Developed in the 1990s to prevent depression relapse, it teaches people to observe their thoughts and feelings without judgment while challenging unhelpful mental habits. Imagine it as mental yoga: stretching your awareness, breathing through discomfort, and letting go of the “what-ifs” that tie your brain in knots.
Here’s the kicker: MBCT isn’t just for calming anxious minds. Research shows it can *physically* reduce tension in the body—including the intricate muscles that control your voice. A 2019 study in the Journal of Voice found that MBCT significantly improved symptoms in patients with muscle tension dysphonia, with one participant joking, “I went from sounding like a haunted house door to my actual self again.”
The Mind-Body-Voice Connection: Science Meets Anecdote
Your voice is a sneakily emotional instrument. Ever tried singing karaoke while anxious? Congrats—you’ve experienced how stress can turn Adele’s “Hello” into a squeaky rendition worthy of a startled mouse. This happens because stress triggers the amygdala (your brain’s drama queen) to activate the “fight-or-flight” response, tensing muscles in your throat, jaw, and diaphragm.
MBCT interrupts this cycle by teaching you to:
1. Notice tension without panicking (e.g., “Hmm, my throat feels tight. Interesting.”).
2. Challenge catastrophic thoughts (“My voice is ruined forever!” becomes “This is temporary; I can soften my muscles.”).
3. Anchor in the present through breath or sensory cues, dialling down the body’s stress response.
Consider James, a teacher who lost his voice every Friday afternoon. Through MBCT, he realized his vocal cords weren’t the problem—his “Sunday Scaries-level dread” of Monday was. By practicing mindful breathing before class and reframing his thoughts (“I don’t need to shout; I can speak with calm authority”), his voice grew stronger, and his students started calling him “The Zen Lecturer.”
But How Do I *Do* It?”: MBCT Tricks You Can Try Today
You don’t need a meditation cushion or a PhD to start benefiting from MBCT. Here are simple strategies to soothe your voice and mind:
1. The 5-Second Body Scan: Close your eyes and mentally “scan” from head to toe. Notice areas of tension (clenched jaw? raised shoulders?). Breathe into those spots, imagining warmth melting the stress away. Pro tip: Do this before speaking engagements—or family Zoom calls.
2. Thought Labeling: When negative thoughts arise (“I sound awful”), tag them like mismatched socks: “Ah, there’s Judgment” or “Hello, Catastrophizing.” This creates mental distance, helping you respond rationally instead of reactively.
3. Mindful Humming: Hum a low, steady note while placing a hand on your throat. Focus on the vibration and any sensations. It’s like giving your vocal cords a massage while grounding yourself in the moment.
A Lighthearted Look at the Evidence
Skeptical? Let’s talk science with a side of humour. A 2021 study had participants with voice disorders practice MBCT for eight weeks. Results showed not just vocal improvement but also reduced anxiety—and one participant cheekily reported, “I finally stopped hissing at my partner during arguments. Now I just mindfully sigh.”
Another trial compared MBCT to traditional voice therapy. Both groups improved, but the MBCT cohort reported something unexpected: better sleep, fewer headaches, and a newfound appreciation for silence. (“Turns out, my voice isn’t a fan of my 24/7 inner monologue about grocery lists,” quipped a participant.)
The Bigger Picture: Why Your Voice Deserves Mindfulness
Voice disorders can feel isolating, but they’re often a signpost pointing to deeper needs: rest, self-compassion, or a break from the mental chatter that exhausts your body. MBCT doesn’t just treat symptoms—it nurtures a kinder relationship with yourself.
As speech-language pathologist Dr. Lisa Thompson notes, “Your voice is your identity. Healing accelerates when clients learn to approach it with curiosity instead of fear. Plus, they stop yelling at their GPS, which is a win for everyone.”
Final Thoughts: Speak Your Truth—Softly, Slowly, and Mindfully
Whether you’re a singer, teacher, or someone who just wants to stop croaking during meetings, MBCT offers tools to harmonize your mind and voice. It’s not a quick fix, but as Sarah (our podcast host) puts it, “I didn’t just get my voice back—I found a steadier, gentler version of myself along the way.”
So next time your voice feels strained, pause. Breathe. And remember: Even the best instruments need tuning. Why not start today?
About the Author: Jane Doe is a speech therapist and mindfulness enthusiast who once tried to cure her stage fright by narrating her grocery list in a British accent. She now helps clients find their voice—without the fake accent.
*Disclaimer*: Always consult a healthcare provider for voice concerns. MBCT is a complementary approach to voice therapy, not a replacement.
**Liked this post? Share it with someone who needs a little more “om” in their vocal cords!** 😊🎤
Finding the Right Speech Therapy in the GTA
Struggling with speech or language? Discover how speech therapy in Toronto, Mississauga, Brampton & online can help. Find an SLP near you & improve communication skills.
Do you have trouble speaking clearly? Does your child struggle with language? You're not alone. Many people in the Greater Toronto Area (GTA) can benefit from speech and language therapy. Speech-language pathologists (SLPs) are trained professionals who can help with various communication and swallowing disorders.
What is Speech-Language Pathology?
Speech-language pathology involves assessing and treating communication and swallowing problems. These problems can arise from various causes, such as developmental delays, stroke, head injuries, or other medical conditions. Speech language pathology treatment aims to improve communication skills and overall quality of life. SLP therapy can address issues with articulation, fluency (stuttering), language, voice, and even cognitive communication.
Where Can You Find Speech Therapy in the GTA?
The GTA offers numerous options for speech therapy. Whether you're looking for speech therapy Mississauga, speech therapy Brampton, speech therapy Etobicoke, or a speech therapist Toronto, you'll find clinics and practitioners ready to help. Many speech language clinics offer services for both children and adults.
Clinics: Many established speech language clinic options exist throughout the GTA. These clinics provide in-person assessments and therapy sessions.
In-Home Therapy: Some providers offer the convenience of in-home speech therapy, bringing services directly to your home, daycare, or school. This can be especially helpful for young children or individuals with mobility issues.
Online Therapy: Speech therapy online is an increasingly popular option, offering flexibility and convenience. Virtual sessions can be as effective as in-person therapy and are suitable for various speech and language disorders.
Finding an SLP Near Me
Searching for an "slp near me" or "speech-language pathologist near me" can feel overwhelming. Here are some tips for finding the right SLP Ontario:
Ask for Referrals: Talk to your family doctor, pediatrician, or other healthcare providers for recommendations.
Check Credentials: Ensure the speech language pathologist ontario is registered with the College of Audiologists and Speech-Language Pathologists of Ontario (CASLPO).
Consider Specialization: Some SLPs specialize in certain areas, such as language therapy, articulation, or fluency disorders. Choose a therapist with experience in your specific area of need.
Virtual Options: Explore virtual speech therapy Canada to conveniently access qualified SLPs from home.
The Importance of Early Intervention
Early intervention is crucial for children with speech and language delays. The earlier a child receives speech and language therapy, the better the outcome. If you have concerns about your child's communication skills, don't hesitate to seek an assessment from a qualified speech language pathologist toronto or elsewhere in the GTA.
Services Offered
SLPs in Toronto and the GTA offer a wide range of services, including:
Speech and language assessments.
Individualized therapy plans.
Articulation therapy.
Fluency therapy (stuttering treatment).
Language therapy.
Voice therapy.
Swallowing therapy.
Parent training and support.
Whether you're seeking speech therapy in Mississauga, speech therapy in Brampton, or any other location in the GTA, remember that help is available. With the proper support, individuals of all ages can improve their communication skills and live more fulfilling lives.
Speech and Hearing Advocacy
In Toronto and beyond, speech therapy bridges gaps in communication, empowering voices of all ages. Whether addressing muscle tension dysphonia at The Voice Clinic, refining s blends for clearer speech, or supporting children with developmental language disorder (DLD), certified professionals (CASLPO/ACSLPA) blend innovation and compassion. Learn how pivotal response treatment, hearing aid advancements (Auracast™), and social communication strategies unlock confidence. Explore the role of orthophonie in Francophone communities, newborn hearing screenings, and ethical standards (HSO). Join the movement for clearer communication—because every voice deserves to be heard.
Celebrating the Power of Speech Therapy: Elevating Communication, Empowering Lives
Communication is the heartbeat of human connection. From a child's first words to a CEO's persuasive pitch, every voice matters. As a profession, speech-language pathology and audiology are dedicated to breaking down barriers, fostering confidence, and unlocking potential—one conversation at a time. Let's explore how this dynamic field transforms lives and why supporting its growth benefits us all.
The Unsung Heroes of Communication
Speech-language pathologists (SLPs), communicative disorders assistants (CDAs), and audiologists are the architects of clearer speech, stronger social skills, and better hearing. Consider these everyday victories:
A teenager with mumbling habits learns to articulate clearly, finally feeling heard by peers.
A professional refining their accent in Toronto gains confidence in boardroom presentations.
A non-speaking child with autism discovers self-expression through PECS (Picture Exchange Communication System)
These moments aren't just "success stories"—they're testaments to the profession's profound impact on dignity, relationships, and opportunity.
Why Speech Therapy Matters More Than Ever
Communication challenges don't discriminate. They affect all ages, backgrounds, and professions. Here's how our field rises to the occasion:
1. Bridging Gaps in Early Development
Early intervention is critical for conditions like developmental language disorder (DLD), speech apraxia, or dyspraxie verbale in French. Research shows that children's speech therapy grounded in play-based methods (like Pivotal Response Treatment) can reshape developmental trajectories. Imagine a toddler who once struggled to say "mama" giggling through a game that strengthens s blends—this is the magic of skilled, compassionate care.
2. Amplifying Voices in Adulthood
Adults face unique hurdles, from muscle tension dysphonia straining a teacher's voice to central auditory processing disorder (CAPD) muddying workplace conversations. SLPs don't just treat symptoms—they empower clients to advocate for themselves through vocal exercises, hearing aid instrument optimization, or strategies for interacting socially with ease.
3. Innovating for the Future
The field thrives on innovation. Think Auracast™ technology turning hearing aids into seamless audio streamers or studies in the Journal of Voice refining treatments for aphonia (complete voice loss). Even AirPods are sparking discussions about accessible hearing solutions! By embracing research and tools like facilitated communication, professionals ensure no one gets left behind.
Standards That Build Trust
Public confidence in speech therapy hinges on rigorous training and ethics. Certifications like the Certificate of Clinical Competence (CCC), oversight by CASLPO and ACSLPA, and adherence to HSO (Health Standards Organization) guidelines guarantee quality care. When you support a profession committed to health standards, you champion:
Accountability in practices like newborn hearing screening and hearing aid fittings.
Ethical approaches to complex cases, such as echolalia or social communication disorder.
Collaboration across languages (e.g., orthophonie in Francophone communities).
Investing in the Profession Benefits Everyone
Advocating for speech therapy isn't just about individual clients—it's about building a society where communication is treated as a human right. Here's how we can all contribute:
Employers: Offer insurance plans that cover speech and language therapy.
Educators: Promote awareness of DLD Awareness Day (October 20).
Communities: Celebrate milestones, whether a child mastering /s/ sounds or an elder rediscovering conversation post-stroke.
Let's Talk About the Future
The profession's potential is limitless. From addressing speech-language salary disparities to expanding OOAQ-certified French-language services in Quebec, there's work to do—and every advocate matters. Whether you're a parent, a colleague, or someone navigating communicative disorders, your voice fuels progress.
Together, we can ensure:
No child is mislabeled as "shy" when they have selective mutism.
No adult resigns themselves to isolation due to mumbling or hearing loss.
Regardless of ability, everyone has the tools to say, "Let's talk."
Join the Movement
Speech therapy isn't just a career—it's a calling to empower, innovate, and connect. Explore #CommunicationForAll or connect with organizations like CASLPO and OOAQ to learn more about the impact of the field.
*Because when we lift the profession, we lift every voice.* 🗣️💙
How to Navigate Speech, OMT and Occupational Therapy in Ontario Without Losing Your Marbles
Navigating Ontario’s speech therapy scene? You’ll need more than poutine and patience. Between decoding rhotacism (wabbit vs. rabbit debates), chasing OAP funding, and tongue-thrusting, this guide serves up dark humour, hockey tickets, and hope.
So, you've decided to buy Guelph Storm tickets to bribe, er, incentivize your kid into surviving another week of speech therapy. Smart move. Nothing says good behaviour like promising hockey games and poutine. But between chasing OAP funding and googling occupational therapy near me at 2 a.m., you've realized this journey is less Mary Poppins and more Lord of the Rings. Let's talk about surviving it—with your sanity intact. #youshallnotpass #balrogsaspets
Step 1: Embrace the Chaos (and the Google Search Bar)
You'll start with noble intentions. "I just need pediatric occupational therapy," you say, sipping Tim Hortons like a champ. Then reality hits: physiotherapy Waterloo? Myofunctional therapy near me? Is this a medical need or a Scrabble board? Suddenly, you're knee-deep in terms like rhotacism (when "rabbit" sounds like "wabbit") and dysarthria (slurred speech, often caused by muscle issues—or, in my case, that third espresso).
You'll find yourself at 2855 Markham Road, staring at a building that looks suspiciously like a former dentist's office. A cheerful therapist will say, "Let's work on social-ability!". At the same time, your child hides under a table, reciting lines from Bluey with the precision of a Shakespearean actor.
Step 2: Decode the Jargon (and the Bureaucracy)
OAP funding: Ontario's autism support version of a golden ticket, except you get massive amounts of paperwork instead of chocolate and Timothy Chalamet in a top hat. You'll learn to write essays titled "Why My Child Deserves Help" while questioning your life choices. Meanwhile, communicative disorders assistant jobs pop up in your LinkedIn feed, tempting you to switch careers. "I could do this!" you think, right before your kid yells, "MOM, ALFIE ATE MY CHEWY TUBE AGAIN." Too bad you don't have a dog.
You'll Google andalusia speech therapy at 3 a.m., wondering if Spain has better answers. They might, and it's a really cool name that makes you crave olives. You also find the Aurora Speech Clinic, where therapists tackle speech th issues (that's "th" as in "thin,"not "th" as in "this is taking forever").
Step 3: Laugh at the Absurdity (Because Crying is Messy, even when it's a laughy-cry; it still makes you puffy)
You'll attend a health care consultation where someone mentions myofunctional therapy near me to fix "mouth breathing"and "tongue thrusting," only to realize you've been mouth-breathing since the early aughts. Oops. #parentalhypocrisy
And let's not forget rhotacism. Yes, your child says "wabbit," but honestly? It's adorable. Until they're 16 and ordering a "wabbit stew" at a fancy restaurant. Wabbits are more prone to myxomatosis than their rhotic kin (see Monty Python's "Rabbit of Caerbannog" for terrifying context).
You'll finally use those Guelph Storm tickets, and as your child cheers, you'll realize the meaning loss you feared—the worry they'd never connect with their peers—is gone. They're here, grounded in the moment, and shrieking with gladiatorial glee, "Fight! Fight! Fight!" (Thanks, social-ability classes.) #overconnected
Final Tip: Keep the Poutine and Popcorn Handy
This journey—through pediatric occupational therapy, dysarthria of speech, and orofacial myofunctional therapy (OMT for those who haven't done a treatment block)—is messy, ridiculous, and occasionally heartbreaking. But you'll survive. When you do, you'll realize the simple effectiveness of Pavlovian training for kids and wonder if it works on husbands, too, as he scarfs the leftover poutine. #chewingwithyourmouthopen #dyinglove
Now, if you will excuse me, I need to google, "Do partially digested chewy tubes hold any residual value?."
TL;DR: Navigating Ontario's speech therapy scene may involve hockey ticket bribes and OAP funding paperwork. Bring snacks, lower expectations, and lean into the chaos. Also, Guelph Voice & Speech Therapy Corp has great parking. Who doesn't love free parking?
Your Voice’s Best Friends: Top 7 Supplements to Keep Your Throat Happy
Your voice is your superpower—don’t let hoarseness or strain hold you back. Explore the 7 essential supplements that singers, podcasters, and heavy voice users swear by to keep their throats happy and voices crystal-clear. Spoiler: Marshmallow root isn’t just for s’mores!
Hey there, vocal rockstar! Your voice is your superpower whether you’re belting high notes, podcasting like a pro, or just *really* good at karaoke nights. But let’s face it—some days, your throat feels more like a sandpaper factory than a well-oiled instrument. You hydrate, warm up, and avoid screaming into the void (mostly), but what if you need a little extra backup? Enter: supplements for vocal health. Not the bland, pill-popping kind, but the wise, strategic allies that’ll keep your pipes smooth, strong, and ready for action. Let’s dive in—no lab coats required.
Why Supplements?
Your vocal cords are delicate little divas. They hate dryness, loathe inflammation, and will throw tantrums if you ignore their needs. While a balanced diet and hydration are VIPs, sometimes life (or a brutal rehearsal schedule) gets in the way. Supplements can fill those gaps, offering targeted support to keep irritation, hoarseness, and those “why do I sound like a frog?” moments at bay. Think of them as your voice’s pit crew.
The A-Team of Vocal Health Supplements
Here’s the lowdown on the top supplements that’ll have your throat singing thank u:
1. Vitamin C: The Immune System’s BFF
What it does: Boosts immunity to fend off colds and throat infections (because getting sick before a gig is a hard pass).
Why singers love it: Less sick days = more stage time. Plus, it’s a natural antioxidant that fights inflammation.
Get it from: Capsules, chewables, or powdered packets stirred into water. Aim for 500–1,000 mg daily, especially during flu season.
2. Zinc: The Sore Throat Slayer
What it does: Shortens cold duration and soothes sore throats. Some studies say it might even protect vocal cords from strain.
Pro tip: Suck on zinc lozenges at the first hint of a tickle. Just don’t overdo it—too much zinc can upset your stomach. We recommend starting with 25mg and take with food.
3. Slippery Elm: Nature’s Throat Coat
What it does: This herb forms a soothing, gel-like layer over irritated throat tissues. Imagine it as a cozy blanket for your vocal cords.
How to use: Look for lozenges or teas. Sip a cup 30 minutes before singing or speaking marathons.
4. Marshmallow Root: Not Just for Campfires
What it does: Like slippery elm, it reduces dryness and irritation. Yes, it’s an actual plant—no sugary campfire treats here!
Bonus: It’s gentle enough for daily use. Try it in tea or capsule form.
5. Omega-3s: Bye-Bye, Inflammation
What they do: These fatty acids (found in fish oil or algae supplements) reduce inflammation, which can help prevent vocal cord swelling.
Singers’ secret: Pair omega-3s with turmeric for a double anti-inflammatory punch.
6. Electrolytes: Hydration’s Wingman
What they do: Help your body hold onto water, lubricating mucous membranes (and your voice).
When to use: After sweating it out on stage or in a hot studio. Look for low-sugar options like coconut water or tablets that dissolve in water.
7. Licorice Root: The Double-Edged Sword
What it does: Soothes sore throats and boosts adrenaline (hello, energy before a show!).
But! Avoid if you have high blood pressure or are pregnant. Always check with your doctor first.
How to Choose Supplements Without Losing Your Mind
Quality matters. Look for brands with third-party testing (NSF, USP). Cheap supplements can be sketchy.
Timing is key: Take slippery elm or marshmallow root on an empty stomach for best absorption. Pair fat-soluble supplements (like omega-3s) with food.
Less is more: Mega-dosing won’t make your voice Mariah Carey-level faster. Stick to recommended amounts.
The “Avoid at All Costs” List
Menthol lozenges: They numb your throat, which can lead to overuse and strain.
Excessive vitamin C or zinc: Too much = stomachaches or worse. Stick to the script.
Alcohol-based tinctures: Drying! Opt for glycerin-based herbal extracts instead.
Final Note: Supplements Aren’t a Solo Act
Even the best supplements can’t replace vocal rest, hydration, or common sense. Use them as part of a bigger toolkit:
Warm up like your career depends on it (because it kinda does).
Sleep more than your cat.
Stress less—yes, anxiety tightens throat muscles. Try meditation or screaming into a pillow (kidding… mostly).
Your Voice Deserves the Spotlight
Think of your vocal cords like a priceless guitar—you wouldn’t let it rust or go out of tune. With the right supplements (and a little TLC), you’ll keep your voice clear, resilient, and ready to wow the crowd. Now go forth, hydrate like a champ, and maybe share that marshmallow root tea with your bandmates. They’ll thank you.
TL;DR: Pop these supplements, not your vocal cords: Vitamin C, zinc, slippery elm, marshmallow root, omega-3s, and electrolytes. Avoid menthol and overdoing it. Your throat will RSVP “yes” to every performance.
Hush Up and Eat: How to Silence Inflammation with Food
Your vocal cords are drama queens. Learn how to shut down inflammation (and its phlegmy entourage) with an anti-inflammatory diet built for singers, podcasters, and anyone who uses their voice like a rented mule. Spoiler: Ditch the sugar, hug the turmeric, and hydrate like your career depends on it. (Spoiler: It does.)
Let’s cut to the chase: your vocal cords are drama queens. One wrong note, a late-night pizza, or a rogue allergen, suddenly they’re staging a coup, leaving you sounding like a broken kazoo. For singers, voice actors, podcasters, and anyone who uses their pipes like a rented mule, inflammation is the ultimate frenemy. It’s why your voice nopes out after three encores or a four-hour Zoom meeting. But fear not, —today, we’re discussing how to eat yourself out of this mess.
Inflammation: The Unwanted Roommate
Inflammation is like that roommate who crashes on your couch, eats your leftovers, and blasts death metal at 3 a.m.—it’s *supposed* to be helpful (thanks, immune system!). Still, when it overstays its welcome, everything goes to hell. Chronic inflammation turns your throat into a scratchy, swollen warzone, which is bad news if your job requires you to sound less like a demonic whisper and more like, well, a human.
But here’s the kicker: you can starve inflammation into submission. Your diet isn’t just fuel; it’s a tactical weapon. Let’s weaponize your grocery list.
Step 1: Ditch the Vocal Cord Arsonists
Before we get to the good stuff, let’s talk about what’s actively trying to ruin you. These foods are the equivalent of pouring gasoline on your vocal cords and lighting a match:
High Fructose Corn Syrup: The Beyoncé of inflammation. It’s everywhere, it’s addictive, and it turns your body into a dumpster fire. Sugar spikes insulin, which triggers inflammatory cytokines (fancy word for “molecular bullies”). If your post-rehearsal snack is a candy bar, you might as well gargle with lava.
Processed Carbs: White bread, pasta, and anything labelled “instant happiness” turns to sugar in your body. Congrats, you’ve just ordered a one-way ticket to Swollen Throat City.
Alcohol: “But red wine is anti-inflammatory!” Cool story. It’s also dehydrating, which turns your mucus membranes into the Sahara. Save the booze for after you’ve nailed your Grammy speech.
Dairy: For some of you, dairy is like inviting a phlegm factory to set up shop in your throat. If milk turns your voice into a mucus-coated mess, swap it for almond/oat/cashew/whatever-milk-Instagram-is-obsessed-with-this-week.
Fried Foods: Trans fats? More like trash fats. They’re linked to inflammation and should be avoided like a telemarketer during dinner.
Step 2: Worship at the Altar of Anti-Inflammatory Foods
Let’s load up on the stuff that’ll make your vocal cords sing hallelujah (or at least stop plotting your demise). These foods are the Avengers of inflammation-fighting:
Turmeric: The Golden God
Turmeric isn’t just a spice; it’s a neon-orange bird flip to inflammation. Curcumin, its active compound, is a potent anti-inflammatory agent. Pro tip: Pair it with black pepper to boost absorption. Add it to soups and smoothies, or mix it into your existential dread—whatever works.
Ginger: Spicy Revenge
Ginger is like turmeric’s hotter cousin who shows up to fight inflammation and then stays for brunch. It’s excellent for soothing sore throats and reducing swelling. Throw it in tea or stir-fries or chew on it raw if you feel masochistic.
Omega-3s: Fishy Business
Fatty fish (salmon, mackerel, sardines) are packed with omega-3s, which tell inflammation to take a hike. Not a fish person? Flaxseeds, chia seeds, and walnuts are your plant-based allies. Just don’t expect them to taste like a salmon sashimi roll.
Berries: Tiny But Mighty
Blueberries, strawberries, and raspberries are loaded with antioxidants that kick inflammation in the teeth. They’re also nature’s candy, so eat them by the handful while muttering, “This is for science.”
Leafy Greens: Popeye Was Ripped for a Reason
Kale, spinach, and Swiss chard are rich in vitamins A, C, and K—all of which help reduce inflammation. If you hate salads, blend them into a smoothie and pretend you drink a green mojito.
Nuts and Seeds: Crunchy Medicine
Almonds, walnuts, and sunflower seeds are packed with healthy fats and magnesium, which help calm inflammation. Just avoid the honey-roasted kind—that’s just sugar in a trench coat.
Step 3: Hydrate or Die-drate
Water is boring. We get it. But dehydration turns your throat into a dry, irritated wasteland, and no amount of vocal warm-ups will save you. Herbal teas (ginger, licorice, chamomile) are your friends. Add honey for its soothing properties, but don’t go Full Winnie-the-Pooh—it’s still sugar.
Pro Hack: Mix warm water with lemon, ginger, and a pinch of turmeric for a throat-soothing elixir. Call it “Voice Saver Soup,” and charge $12 a cup at your next gig.
Step 4: Meal Ideas for People Who Hate Cooking
Breakfast: Overnight oats with chia seeds, almond milk, and berries. Top with walnuts. Yes, it’s basic, but so are yoga pants. Look at how that turned out.
Lunch: A quinoa bowl with roasted veggies, avocado, and a turmeric-ginger dressing. Instagram it #WellnessWarrior.
Dinner: Baked salmon with steamed greens and sweet potatoes. Bonus points if you eat it while humming scales.
Snacks: Apple slices with almond butter, carrot sticks with hummus, or a handful of mixed nuts. Avoid the vending machine—it’s a trap.
Step 5: Supplements for the Lazy (But Committed)
If chewing actual food feels like too much work, try these:
Curcumin supplements (with black pepper extract).
Omega-3 capsules (fish oil or algae-based).
Zinc lozenges for immune support (but don’t overdo it—zinc can be a diva).
The Bottom Line
Your voice is your moneymaker, art, and/or emotional support instrument. Treat it like a luxury car, not a rental Dodge Neon. Ditch the inflammatory garbage, load up on the good stuff, and hydrate like you’re training for a hydration marathon.
And remember: when your vocal cords are happy, you can return to doing what you do best—making noise, getting paid, and annoying the neighbours.
Now go eat a salad, you magnificent siren.
TL;DR: Sugar bad. Turmeric good. Drink water. Your voice isn’t going to save itself.
How to Get Approved for the Disability Tax Credit
Navigating the T2201 form is essential for claiming Canada’s Disability Tax Credit. Our guide simplifies eligibility, completing the form with a medical practitioner, and CRA’s review process. Unlock tax relief and financial support for disabilities.
Understanding the T2201 Form for Disability Tax Credit
Navigating the world of taxes can be daunting. It becomes even more complex when dealing with disability tax credits.
Enter the T2201 form, also known as the disability tax credit form.
This form, the Disability Tax Credit Certificate, is a crucial document for Canadians with disabilities. It's the gateway to accessing the Disability Tax Credit.
However, understanding the T2201 form can be a challenge. There's much to grasp, from eligibility criteria to application.
This guide aims to simplify that process. We'll break down the T2201 form for access to the Revenue Canada disability tax credit, helping you understand its purpose, how to fill it out, and how to maximize its benefits.
Whether you're an individual with a disability, a caregiver, or a tax professional, this guide is for you. Let's demystify the T2201 form together.
What is the T2201 Form?
The T2201 form is vital in accessing tax benefits for individuals with disabilities in Canada. Officially termed the Disability Tax Credit Certificate, it serves as the primary paperwork to claim this particular tax credit.
This form is crucial for reducing the amount of income tax owed. By qualifying for the Disability Tax Credit, eligible individuals or their supporting family members can benefit from significant tax relief.
Completing the T2201 tax form involves more than just filling in personal details. It requires a comprehensive assessment of the disability's impact on the individual's daily activities. The goal is to establish eligibility by demonstrating a prolonged and significant impairment.
Additionally, the form helps to align with other benefits and support systems. Proper completion of the form T2201 can lead to further financial aid through various government programs, making it a valuable document beyond income tax reductions.
Understanding the T2201 form's significance is the first step in streamlining the process and ensuring eligible Canadians receive the financial support they are entitled to. It's a powerful tool designed to alleviate some financial burdens associated with living with a disability.
Who is Eligible for the Disability Tax Credit?
Eligibility for the Disability Tax Credit hinges on specific criteria. The primary focus is on individuals who experience prolonged and severe impairments. These impairments must noticeably restrict everyday activities.
The type and nature of the impairment play a crucial role. It must last or be expected to last for at least 12 months. A thorough evaluation of its impact on daily functioning is essential.
The restrictions can manifest in various ways. They might significantly limit someone in walking, speaking, hearing, or performing mental functions necessary for everyday life. It also covers impairments requiring life-sustaining therapy at least three times weekly.
While the specific details can vary, the overarching criterion is consistent. The disability must have a marked and prolonged effect on the individual's ability to perform daily activities. This ensures the credit targets those most in need.
A qualified medical practitioner must certify these conditions on the T2201 form. Their involvement legitimizes the claims and affirms that the individual's condition meets the prescribed standards for eligibility.
The Role of Qualified Practitioners in Certifying the T2201
Qualified practitioners play a pivotal role in the T2201 form certification. They assess the individual's medical condition thoroughly. Their expertise helps ensure the eligibility criteria are met accurately.
These practitioners can include physicians, psychologists, or occupational therapists. Their involvement is crucial because they provide the necessary documentation. This documentation confirms how the impairment affects daily living.
Their assessment is not a mere formality. It involves a detailed evaluation. Practitioners must determine the severity and duration of the impairment, supporting the individual's claim with evidence.
By certifying the T2201 form, these professionals help streamline the application process. They also reduce the risk of errors or omissions. Their input is integral to securing the Disability Tax Credit for eligible individuals, helping them access vital financial support.
Step-by-Step Guide to Completing the T2201 Form
Filling out the T2201 form might seem daunting at first. However, breaking it down step-by-step can simplify the process. Remember, accuracy is key to avoid delays or denials.
Start by downloading the form from the Canada Revenue Agency (CRA) website. It's available in both PDF and print formats. Choose the version that suits your preference.
Next, read the instructions carefully. Each section comes with clear guidelines. Taking the time to understand them ensures your information is accurate.
Proceed to fill in your details. This includes your name, address, and social insurance number. Double-check for any typos or errors.
The following section requires detailed medical information. Coordinate with your qualified practitioner for this part. They'll provide the necessary medical details and certification.
Make sure your practitioner completes their section fully. This includes their signature and relevant contact information. Incomplete forms might lead to rejection.
Once the medical section is complete, review the entire form. Look for any blank fields or inconsistencies. It's crucial to ensure everything is filled out correctly.
After reviewing, sign the form. Your signature finalizes and validates your application. Without it, your submission remains incomplete.
Gather any additional documents that might support your application. Although not always required, further documents can help confirm your claim.
Checklist for Completing the T2201 Form:
Download the T2201 form from the CRA website.
Review all sections and instructions thoroughly.
Fill in personal information accurately.
Coordinate with a qualified practitioner for medical sections.
Ensure practitioner details and signature are complete.
Review and sign the completed form.
Gather supporting documents if necessary.
Finally, keep copies of the completed form and any supporting documents. You'll need them for future reference. A duplicate set is also helpful in case any issues arise later.
Submitting the T2201 Form to Revenue Canada
After completing the T2201 form, the next step is submission. This is a crucial part of the process. Ensure you send the form to the right place.
You can mail the completed form to the Canada Revenue Agency. Be sure to use the address provided in the instructions on the form. It's important to double-check the mailing address to avoid misdelivery.
Alternatively, you can submit electronically through CRA's My Account online service. Submitting online is faster and confirms receipt. This method is ideal for those seeking quick processing.
Keep track of your submission date. Knowing when you sent the form can help in case any delays or follow-ups are needed. It's advisable to retain a copy of your submission for your records. Keeping accurate records ensures you have proof of submission.
Understanding the Review Process by the CRA
A thorough review begins once the Canada Revenue Agency receives your T2201 form. This process is essential for determining your eligibility. The CRA ensures all details comply with their requirements.
The review involves examining the medical certification provided by a qualified practitioner. They check for accuracy and completeness. If there are uncertainties, they may request additional information.
Processing times vary, so patience is necessary during this stage. It's not unusual for the CRA to take several weeks to complete their assessment. In the interim, consider monitoring the status through your CRA My Account.
After the review, the CRA will inform you of the outcome. You will receive a notice of determination, which explains the decision. If approved, you will receive a disability tax certificate. The benefits can significantly reduce your taxable income. If denied, it sets the stage for potential appeals or adjustments.
How the Disability Tax Credit Affects Other Government Programs
The Disability Tax Credit (DTC) can influence your eligibility for various government programs. Being approved for the DTC may open doors to additional benefits. These benefits might include other tax credits or financial aid.
Some programs require DTC approval as a qualifying criterion. Therefore, accessing the credit can broaden your resource options. It serves as a gateway to further support.
However, it's crucial to understand the interactions between programs. Some benefits may be mutually exclusive or affect program eligibility thresholds. Staying informed on these nuances ensures you make the most of available resources.
Common Misconceptions and Tips for a Smooth Application
The T2201 form can seem daunting due to common misconceptions. Many believe it's only for severe disabilities. In reality, various conditions qualify.
Another misconception is that approval is guaranteed. Each application undergoes a detailed review. Ensuring accuracy and completeness is crucial.
It's vital to understand the role of qualified practitioners. Their input is not just a formality; it's essential for validation. A clear, comprehensive assessment strengthens your application.
To avoid delays and rejections, follow these tips:
Double-check that all sections of the form are completed.
Ensure the supporting medical documents are current.
Communicate clearly with your practitioner about your condition.
Be honest and precise in all descriptions.
Keep copies of all correspondence for your records.
Missteps in the application can be costly, both time-wise and financially. With diligent preparation and understanding, the process can be much smoother. Taking these steps increases your chance of a successful claim.
Appealing a CRA Decision and Adjusting Previous Tax Years
Navigating a CRA decision can be daunting, especially if your Disability Tax Credit claim is denied. The first step is understanding their decision letter. It will provide specific reasons for the denial, which is crucial for a successful appeal.
Appealing involves a formal objection. This must be filed within 90 days of the CRA's decision. A detailed explanation, along with additional supporting documents, strengthens your case.
During the appeal process, patience is vital. The review may take time, depending on the complexity of your case. Keeping records of all communications is essential.
If your appeal is successful, you might be eligible to adjust previous tax years. This can result in additional refunds. The CRA allows claims retroactively, up to ten years.
Consulting a tax professional or advocate can be beneficial. They can provide guidance and ensure all necessary steps are taken. This can enhance the likelihood of a favourable outcome.
Conclusion: The Importance of the T2201 Form
The T2201 form is pivotal in securing the Disability Tax Credit. This credit lightens the tax burden for individuals with disabilities and their families.
Filing the form accurately opens doors to significant financial support. It enhances quality of life by reducing out-of-pocket expenses related to disabilities.
Understanding and effectively utilizing the T2201 form extends beyond tax savings. It contributes to economic empowerment and independence for individuals facing disabilities. By fostering awareness, it supports an inclusive and equitable society.